Therapeutics based on immune system modulation have been used to treat infectious illnesses and cancer. Antibodies that block programmed cell death protein 1 (PD-1) and programmed cell death-ligand 1 (PD-L1) have shown therapeutic effectiveness in various oncological conditions. These treatments have transformed cancer treatment.
Cancer drugs that activate the immune system to target tumors are a promising treatment option for many forms of cancer. However, some of these medications cause excessive systemic inflammation when delivered through the vein, making them dangerous to patients.
A new study from MIT researchers shows that when immunostimulatory prodrugs inactive drugs that must be activated in the body are tuned for optimal activation timing, the drugs stimulate the immune system to attack tumors without the side effects associated with the active form of the drug.
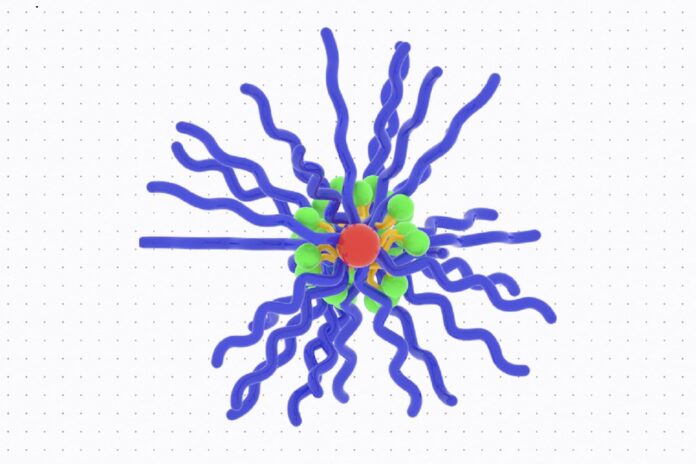
The researchers created prodrugs with bottlebrush-like structures based on a family of chemicals known as imidazoquinolines (IMDs). Mice given these prodrugs with optimized activation kinetics experienced a considerable reduction in tumor development with no adverse effects.
The researchers expect that by combining this method with other immunotherapy medications or cancer vaccines, they may be able to increase immune system responses in cancer patients.
Sachin Bhagchandani, an MIT graduate student who is the study’s lead author, said, “Our bottlebrush prodrug library enabled us to show an immunological effect of controlling immunotherapy kinetics, allowing us to boost immune responses while minimizing the side effects. This approach opens up avenues for scientists who want to decouple toxicity from some promising immunotherapy agents.”
The organic molecules known as IMDs connect to Toll-like receptors located on macrophages and other innate immune system cells. When activated, these cells release cytokines and other inflammatory molecules.
The FDA approved topical IMD medicines to treat some forms of skin cancer in 1997. However, none were approved because the treatments caused too much systemic inflammation.
The MIT researchers wanted to see if prodrugs of IMDs, which are inactive until turned “on” in the tumor microenvironment, could help lessen such negative effects.
Johnson’s lab has recently produced a novel sort of prodrug platform structured like a bottlebrush, consisting of chains extending from a central backbone, giving the molecule a bottlebrush-like structure. Cleavable linkers that define the rate of active IMD release bind inactivated drugs along the bottlebrush backbone.
To study how prodrug activation kinetics affect antitumor responses, the researchers created and tested six bottlebrush prodrugs that differed only in their release rate. The researchers anticipated that bottlebrush prodrugs could deliver active IMDs to tumors while preventing release into the bloodstream.
Johnson said, “Our ability to synthesize six bottlebrush prodrugs with identical sizes and shapes uniquely allows us to isolate and study release kinetics as a key variable. Excitingly, we find that it is possible to identify prodrug structures that limit IMD exposure to the whole body, thereby avoiding toxicity, and that activate in tumors to give antitumor efficacy.”
In preliminary tests in cells and animals, the fastest-acting prodrugs caused immune-related side effects such as weight loss and higher cytokine levels. However, neither the medium- nor slow-release variants produced these results.
The researchers examined the IMD bottlebrush prodrugs in two separate animal models of colon cancer. The prodrugs accumulated efficiently in tumors and were taken up by innate immune cells, where their linkers were cleaved. When active IMDs are released, immune cells release cytokines and other chemicals, which activate neighboring T cells to attack the tumor. Tumour growth was dramatically reduced in mice treated with the prodrugs in both scenarios. Tumors were eliminated in roughly 20% of the mice when paired with a checkpoint-blocking inhibitor.
Mice given resiquimod bottlebrush prodrugs did not exhibit any of these effects. However, mice treated with the IMD utilized in this work, known as resiquimod, displayed weight loss, raised cytokine levels, and decreased white blood cell count, as expected.
Bhagchandani said, “Our molecules were able to safely reduce these effects by controlling how much of the active drug is released in the blood. If you minimize the release of the active compound there, then you’re able to get antitumor effects at the tumor site without the systemic side effects.”
According to a new study, the most potential application for IMD bottlebrush prodrugs could be in combination with another drug that enhances the immune response or as adjuvants to enhance the immune system’s response to cancer vaccines.
Irvine said, “The ability of the bottlebrush prodrug strategy to change both where the drug accumulates in the body and when it is active is very attractive for activating immune responses against cancer or another disease safely.”
This research was funded by the Marble Center for Cancer Nanomedicine, the Ragon Institute, the Koch Institute Frontier Research Program, and the National Cancer Institute.
Journal Reference:
- Bhagchandani, Spranger, Irvine, et al. Engineering kinetics of TLR7/8 agonist release from bottlebrush prodrugs enables tumor-focused immune stimulation. Science Advances. DOI: 10.1126/sciadv.adg2239