A new study has found that recently discharged patients with Coronavirus produce virus-specific antibodies and T cells.
It remains unclear why immune responses generally varied over the patients. According to scientists, this variability might be identified with the initial quantities of virus that the patients experienced, their physical states, or their microbiota.
Other open inquiries include whether these immune responses secure against COVID-19 upon re-exposure to SARS-CoV-2, just as which sorts of T cells are activated by contamination with the virus. It is likewise imperative to take note of that the lab tests that are utilized to recognize antibodies to SARS-CoV-2 in people still need further validation to decide their precision and reliability.
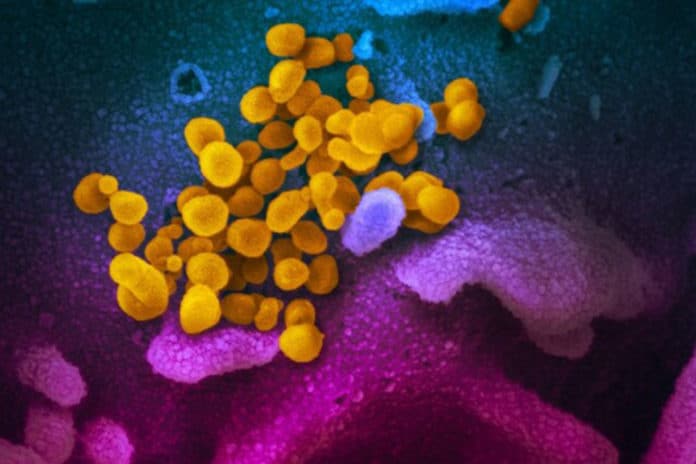
Scientists collected blood samples from COVID-19 patients who have recently become virus-free and, therefore, were discharged and detected SARS-CoV-2-specific humoral and cellular immunity in 8 newly discharged patients. Follow-up analysis on another cohort of 6 patients two weeks post-discharge also revealed high titers of IgG antibodies. In all 14 patients tested, 13 displayed serum neutralizing activities in a pseudotype entry assay. Notably, there was a strong correlation between neutralization antibody titers and the numbers of virus-specific T cells.
Co-senior study author Chen Dong of Tsinghua University said, “These findings suggest both B and T cells participate in immune-mediated protection against the viral infection. Our work has provided a basis for further analysis of protective immunity and for understanding the mechanism underlying the development of COVID-19, especially in severe cases. It also has implications for designing an effective vaccine to protect against infection.”
Compared to healthy controls, both newly discharged and follow-up patients showed higher levels of IgM and IgG antibodies that bind to the SARS-CoV-2 nucleocapsid protein, which encapsulates the viral genomic RNA, as well as the S protein’s receptor-binding domain (S-RBD), which binds to receptors on host cells during the process of viral entry. Taken together, these findings show that COVID-19 patients can mount antibody responses to SARS-CoV-2 proteins and suggest that these antibodies are maintained for at least two weeks after discharge.
Likewise, five recently released patients had high concentrations of neutralizing antibodies that bind to a pseudovirus expressing the SARS-CoV-2 S protein. Neutralizing antibodies prevent infectious particles from interfacing with host cells. Likewise, all except one follow-up patient had detectable neutralizing antibodies against the pseudovirus.
Compared to healthy controls, five newly discharged patients had higher concentrations of T cells that secrete interferon-gamma (IFNγ) – a signaling molecule that plays a critical role in immunity—in response to the SARS-CoV-2 nucleocapsid protein.
These are the same patients who had high concentrations of neutralizing antibodies. Also, three newly discharged patients showed detectable levels of IFNγ-secreting T cells specific to the SARS-CoV-2 main protease—a protein that plays a critical role in viral replication.
Meanwhile, seven newly discharged patients showed detectable levels of IFNγ-secreting T cells specific to the S-RBD of SARS-CoV-2. By contrast, only one follow-up patient had a high concentration of IFNγ-secreting T cells responsive to the nucleocapsid protein, the main protease, and S-RBD.
Co-senior study author Fang Chen of Chui Yang Liu Hospital affiliated to Tsinghua University said, “Our results suggest that S-RBD is a promising target for SARS-CoV-2 vaccines. But our findings need further confirmation in a large cohort of COVID-19 patients.”
Journal Reference:
- Detection of SARS-CoV-2-specific humoral and cellular immunity in COVID-19 convalescent individuals. DOI: 10.1016/j.immuni.2020.04.023