Researchers from the Knight Initiative for Brain Resilience at Wu Tsai Neuro of Stanford University have found a surprising link between brain cells that help create insulation around nerve fibers, our sleep patterns, and neurodegenerative diseases like multiple sclerosis (MS).
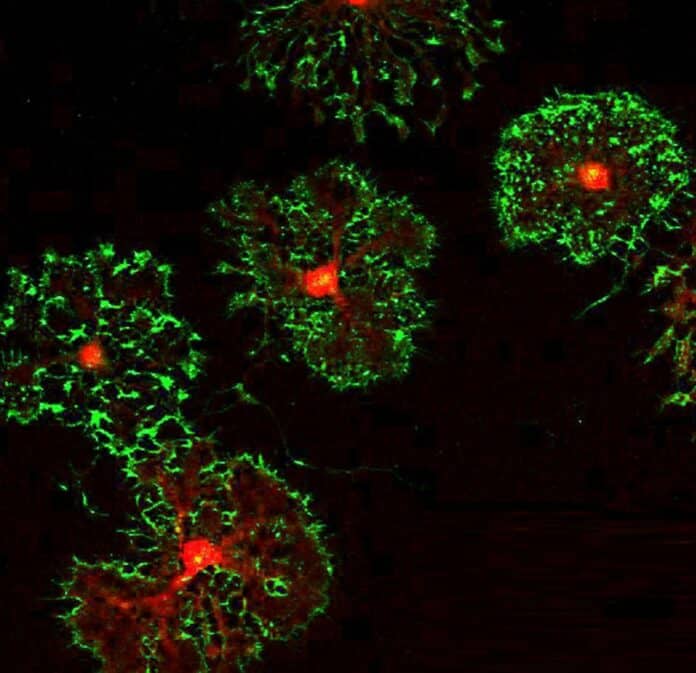
The cells they studied are called oligodendrocyte precursor cells (OPCs). These cells can eventually become oligodendrocytes, which produce myelin – the protective layer around nerve fibers that helps transmit signals in the brain. However, OPCs have various functions before becoming oligodendrocytes, including roles in the immune system and even forming connections with neurons.
Erin Gibson, an assistant professor of psychiatry and behavioral sciences and lead author of the new work, said, “To me, OPCs are the most interesting cell in the central nervous system, partly because, in many ways, they can act like all the other cells in the central nervous system.”
The paper, published on August 31st in Neuron, had Daniela Rojo, a Brain Resilience Scholar supported by the Knight Initiative, as the first author. In this study, Gibson, Rojo, and their team discovered that OPCs may have a surprising connection to sleep, which could be crucial for brain health, particularly for night shift workers.
As a circadian biologist, Gibson understood how our body’s internal clock affects various functions. He wondered if glial cells, like OPCs, might also have their daily rhythms. Their research confirmed that OPCs have circadian rhythms, with about 10% of their genes following a 24-hour cycle. This is the first evidence that the circadian system strongly influences OPCs.
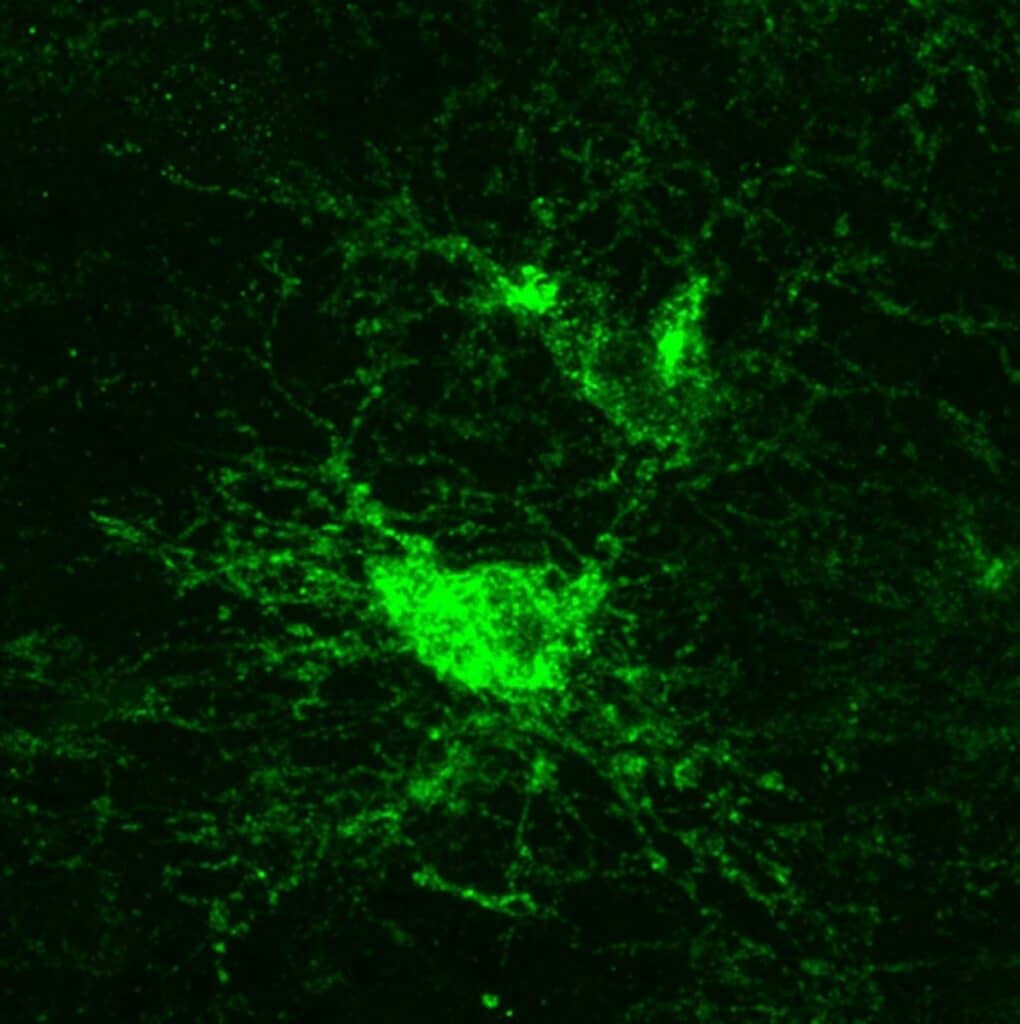
Gibson and Rojo’s team found that when the circadian regulation of OPCs is disrupted, it has adverse effects. This disruption affects both sleep patterns and the health of the myelin, which insulates neurons. When a critical circadian gene called Bmal1 was removed in OPCs, the cells didn’t divide and function properly. They also didn’t move to where they were needed in the brain and looked abnormal.
These changes in OPCs led to reduced myelin insulation and impaired myelin repair after injuries. The effects were most severe when Bmal1 was removed during embryo development, showing its importance in brain development.
The impaired myelination affected the mice’s cognitive abilities and movement. Mice without Bmal1 had trouble with attention tasks and moved more slowly when walking.
The research team was particularly interested in how messed-up OPCs affected sleep. In mice, they found it more challenging to stay in a deep, non-REM sleep, leading to more naps during their active phase when they should be awake. This increased daytime napping is considered one of the early signs of Alzheimer’s disease.
Curious about whether this sleep problem might be linked to other neurodegenerative diseases, they looked at human genetic data. They discovered that sleep fragmentation, a type of sleep deficit, was associated with a higher risk of developing multiple sclerosis (MS).
This led them to consider that the greater risk of MS might be connected to the finding that mice with OPCs lacking the Bmal1 gene struggled to repair myelin after a demyelinating injury. In simpler terms, disruptions in sleep patterns, such as those in night shift workers, might increase the risk of demyelinating disorders like multiple sclerosis.
The researchers are still figuring out whether the problems with myelination and sleep in mice were due to the absence of Bmal1 in the cells, its impact on myelin, or if another gene might be involved. They’re conducting more experiments to understand how Bmal1 regulates OPCs more precisely.
However, if the disruption of OPCs by Bmal1 loss does lead to similar issues in humans and plays a role in diseases like MS, it could become a new target for treatments in the future.
Daniela Rojo said, “We haven’t done a great job developing drugs that target an enhancement in oligodendrogenesis and remyelination. This tells us that this is a new molecular pathway that plays a role in how these OPCs proliferate, differentiate, and migrate into lesions. And so if we can target it, maybe we might be able to make that process more efficient.”
Furthermore, Gibson suggests their findings might open the door to a “chronotherapeutic” approach for conditions like MS that affect myelin. This means existing drugs targeting oligodendrocytes could be more effective if administered at specific times of the day.
In their future research, Gibson aims to dive deeper into the reasons behind the sleep changes they observed and determine if other myelin-related issues also lead to sleep problems.
These results open new avenues for understanding the relationship between circadian rhythms, myelin health, and neurodegenerative diseases. Additionally, the research hints at the potential for chronotherapeutic approaches in treating conditions that affect myelin, such as MS.
Journal reference:
- Daniela Rojo, Louisa Dal Cengio etal., BMAL1 loss in oligodendroglia contributes to abnormal myelination and sleep. Neuron. DOI: 10.1016/j.neuron.2023.08.002.