In Alzheimer’s disease (AD), dysfunctional mitochondrial metabolism is associated with synaptic loss, a major pathological factor in cognitive decline. A team from Scripps Research has identified the energetic reactions in brain cells that malfunction and lead to neurodegeneration.
Using a small molecule to address the malfunction in the mitochondria, the cell’s primary energy producers, the researchers successfully restored many neuron-to-neuron connections in nerve cell models derived from human Alzheimer’s patient stem cells. These findings suggest that improving mitochondrial metabolism could be a promising therapeutic target for Alzheimer’s and related disorders.
Senior author Stuart Lipton, MD, Ph.D., Step Family Foundation Endowed Professor and Co-Director of the Neurodegeneration New Medicines Center at Scripps Research, and a clinical neurologist in La Jolla, Calif said, “We thought that if we could repair metabolic activity in the mitochondria, maybe we could salvage the energy production. In using human neurons derived from people with Alzheimer’s, protecting the energy levels was sufficient to rescue many neuronal connections.”
In a recent study, the researchers led by Dr. Lipton identified a block in the enzymes responsible for energy production due to an abnormal tag of nitrogen (N) and oxygen (O) atoms onto a sulfur (S) atom, forming a dysfunctional “SNO” enzyme. This reaction, known as S-nitrosylation, and the team demonstrated that a virtual “SNO-Storm” of these reactions occurred in the Alzheimer’s brain neurons.
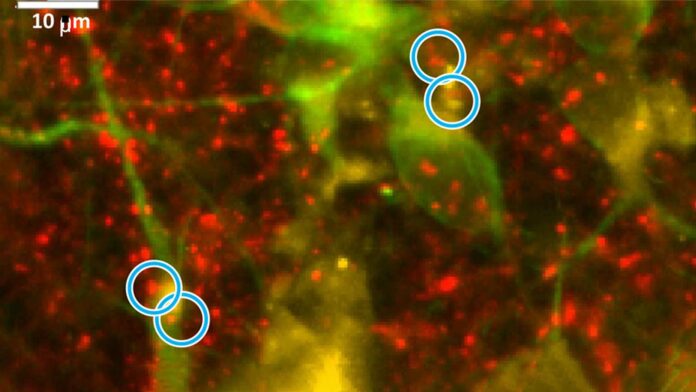
The researchers made this discovery by comparing human brains obtained from people with Alzheimer’s disease to those without brain disease. They then generated nerve cells from stem cells derived from skin biopsies of individuals with and without a genetic mutation causing Alzheimer’s. They calculated cellular energy production using metabolic labels and an oxygen-measuring apparatus and identified deficits in Alzheimer’s nerve cells compared to controls.
The study revealed a disrupted Krebs cycle, a cellular process in mitochondria that produces ATP, the body’s crucial molecular power source. The researchers identified a bottleneck in forming a key molecule, succinate, which hinders ATP production.
The bottleneck impairs mitochondria’s ability to generate energy to sustain neurons and their connections. To address this, the researchers supplied missing succinate molecules, restoring energy production and repairing a significant portion of lost synapses in Alzheimer’s neurons.
Lipton said, “Succinate is not a compound that people can now take as a treatment, but it’s proof-of-principle that you can re-energize the Krebs cycle. The beauty of the study is that we were able to show this in living nerve cells derived from Alzheimer’s patients, but we still have to come up with a much better compound to develop an effective drug for humans to take.”
Journal Reference:
- Alexander Y. Andreyev, Hongmei Yang, Paschalis-Thomas Doulias, Nima Dolatabadi, Xu Zhang, Melissa Luevanos, Mayra Blanco, Christine Baal, Ivan Putra, Tomohiro Nakamura, Harry Ischiropoulos, Steven R. Tannenbaum, and Stuart A. Lipton. Metabolic Bypass Rescues Aberrant S-nitrosylation-InducedTCA Cycle Inhibition and Synapse Loss in Alzheimer’sDisease Human Neurons. Advanced Science. DOI: 10.1002/advs.202306469