Fragile X syndrome, a common inherited intellectual disability, might affect brain cells before a child is born. Usually, it’s diagnosed at the age of 3 or later. A recent study from the University of Wisconsin–Madison found that a protein called FMRP, lacking in people with fragile X syndrome, plays a role in how mitochondria work during prenatal development.
Mitochondria are like power plants in our cells. This discovery changes how we think about the early causes of Fragile X syndrome and offers hope for potential treatments to help damaged brain cells.
A team of researchers, including postdoctoral fellows Minjie Shen, Carissa Sirois, Yu (Kristy) Guo, and Meng Li, working with Professor Xinyu Zhao, a neuroscientist at UW–Madison’s Waisman Center, made a discovery. They found that a protein called FMRP helps control a gene called RACK1, which is essential for the function of mitochondria, the cell’s power plants. Using a drug to improve mitochondrial function, they managed to repair brain cells harmed by the lack of FMRP.
Fragile X syndrome (FXS) can cause a person’s development delays, like not sitting, walking, or talking when they should. It can also lead to various levels of intellectual disability, learning issues, and social and behavioral problems. Many individuals with FXS are also diagnosed with autism spectrum disorder.
In earlier research, Zhao found that their mitochondria were smaller and unhealthy in mice with a deficiency of FMRP, which mimics FXS. They also found that FMRP controls genes involved in a process where mitochondria fuse to produce more energy for cells.
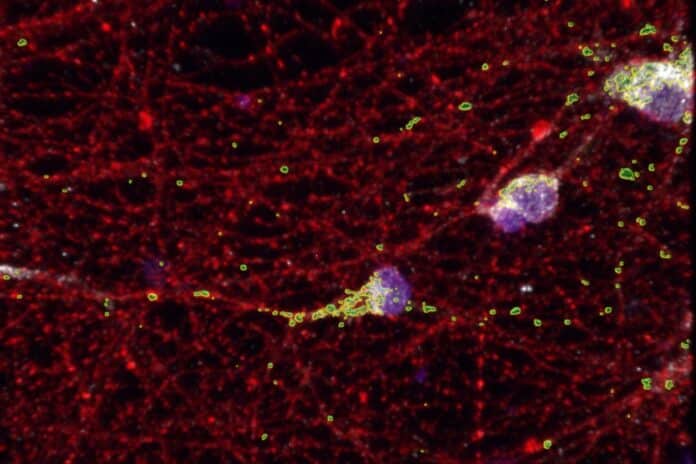
In this study, the researchers grew brain cells, known as neurons, from induced pluripotent stem cells. These stem cells came from people with FXS, which allowed the researchers to study the disorder at the cellular level. They wanted to see if the mitochondria in human cells had the same problems as those in mice.
Zhao said, “We found that human neurons also have fragmented (smaller) mitochondria. In human neurons, it’s a deficit in twofold. Not just fission-fusion, but also likely in the production of mitochondria.”
Furthermore, they observed a reduced number of mitochondria in neurons that originated from individuals with FXS, a phenomenon not present in the neurons of the FXS-modeling mice.
While it’s been known for a while that FMRP plays a significant role in Fragile X Syndrome (FXS), this discovery shows that it’s also involved in the condition’s early stages.
FXS symptoms typically appear well after a baby is born. Many babies seem to develop normally at first but then start showing signs of slower development, autism-like features, or other developmental problems. Most children with FXS are diagnosed at three years old or even later.
This finding challenges the idea that FMRP is mainly crucial for later stages of development. FMRP is a protein that regulates messenger RNA, like a copy of DNA used to make the proteins that do things in our cells.
The researchers found that many of these messenger RNAs that FMRP interacts with are linked to autism, creating a connection between FXS and autism spectrum disorder. Surprisingly, many of these messenger RNAs are controlled by superactive genes during prenatal development but less so after birth.
Zhao said, “FMRP has a function in prenatal development that we have not thought about before. The fact that we found that FMRP also regulates prenatal development is fascinating. It is indicating that what we see in fragile X syndrome, some of the effects already happened within the prenatal development.”
In their study, the researchers identified a critical gene called RACK1, which had never been linked to FXS before. They found that when RACK1 levels are low in fragile X neurons, the mitochondria (the cell’s powerhouses) don’t work well, and the neurons behave like immature ones, becoming overactive. However, when they added more RACK1, it fixed these issues.
The researchers screened drugs on neurons from individuals with FXS and found a medicine called leflunomide that improved mitochondrial problems. This treatment enhanced the mitochondria and reduced the overactivity in the neurons.
Next, they plan to examine the mitochondrial problems in more detail and determine which essential proteins are lacking in FXS-affected neurons. They also aim to understand how RACK1 and leflunomide work to fix mitochondrial function.
Journal reference:
- Minjie Shen, Carissa L. Sirois., et al., Species-specific FMRP regulation of RACK1 is critical for prenatal cortical development. Neuron. DOI: 10.1016/j.neuron.2023.09.014.