Newborns in Uganda are facing a grave threat as researchers have recently confirmed the presence of a new bacterial strain responsible for a significant rise in deaths and disease. This alarming discovery has raised concerns about the health and well-being of infants across the country.
The research findings highlight the urgent need for immediate attention and practical strategies to combat this deadly bacterial strain and protect the vulnerable newborn population in Uganda.
In 2007, at Yale University, pediatric neurosurgeon Steven Schiff, MD, Ph.D., witnessed a distressing situation at the CURE Children’s Hospital in Uganda. Mothers arrived daily, carrying infants with enlarged heads, desperately seeking a cure. These babies had all been born healthy but developed severe infections within weeks. As they recovered, their heads started rapidly enlarging due to postinfectious hydrocephalus, a devastating condition caused by an abnormal buildup of cerebrospinal fluid in the brain’s ventricles.
With no known cure, the pressing need for neurosurgery to alleviate the harmful pressure on the brain became a global concern, particularly in East Africa, where Uganda alone faced approximately 4,000 new cases each year. Limited access to advanced care resulted in high mortality rates. At the same time, even those reaching the CURE Children’s Hospital struggled to recover due to the existing damage caused by the infection.
This heartbreaking situation motivated Dr. Schiff to advocate for increased awareness and action to address newborn infections in developing countries, emphasizing the vulnerability of infants lacking political voices.
After 16 years of relentless investigation, the team finally published a groundbreaking paper in the Lancet Microbe on June 19, 2023. Based on three interconnected research projects, the study pinpointed the Paenibacillus thiaminolyticus bacteria as the culprit behind postinfectious hydrocephalus in Uganda.
Dr. Sarah Morton, co-lead author and assistant professor of pediatrics at Harvard Medical School, hails these results as the culmination of decades of collaboration, providing a promising pathway for targeted diagnosis and treatment of Paenibacillus infections.
This discovery marks a significant breakthrough in unraveling the mystery that had confounded researchers, given the challenges posed by limited resources, difficulties in sample preservation, and the unavailability of advanced sequencing technologies in Uganda. Driven by their determination to find answers, Dr. Schiff and his colleagues pursued the solution, firmly believing that the puzzle could be solved.
Schiff says, “The NIH Director’s high-risk, high-reward programs took a risk on us, and we never could have brought the teams together and cracked this mystery properly if they had not given us this chance.”
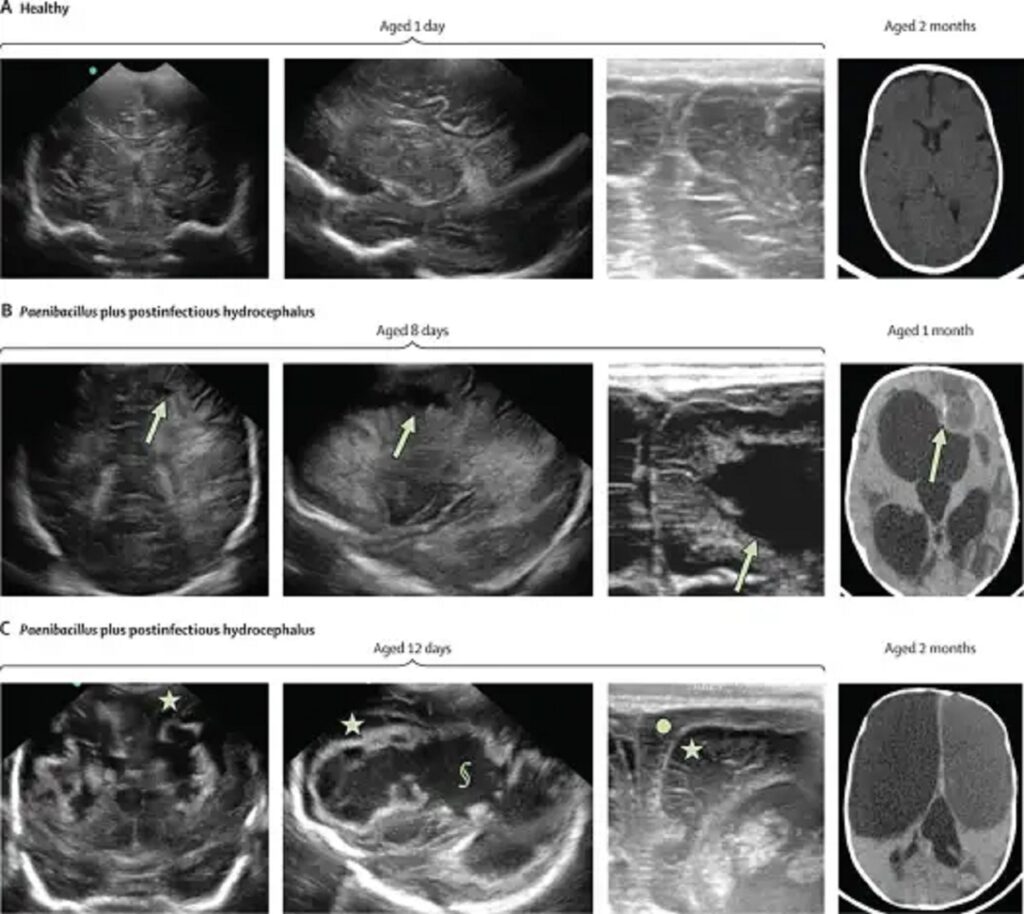
In a remarkable collaboration, Schiff’s team of researchers identified Paenibacillus thiaminolyticus as the previously underestimated organism swimming in Ugandan infants’ hydrocephalus brains. They successfully cultured some strains of this bacterium, discovering its resistance to commonly used antibiotics and the presence of a highly lethal toxin. Publishing their findings in Science Translational Medicine in 2020, the team embarked on further investigations to determine the source and role of the bacteria in postinfectious hydrocephalus cases.
Although maternal trials and examinations of newborns with serious infections revealed no evidence of maternal transmission, Paenibacillus was confirmed in 6% of newborns with sepsis. Astonishingly, 44% of postinfectious hydrocephalus cases showed PCR confirmation of Paenibacillus infection.
The team’s PCR tests further demonstrated that the same bacteria caused the newborn infection and subsequent hydrocephalus. These groundbreaking findings identify the bacterium responsible for most infections in Ugandan children and open doors for exploring prevention and treatment strategies for Paenibacillus infections.
Landmark studies published in the Lancet Microbe and Clinical Infectious Disease established Paenibacillus as the previously overlooked culprit behind the widespread hydrocephalus and infant mortality cases.
The research highlights the importance of recognizing Paenibacillus as a significant cause of neonatal infections, as commonly used antibiotics often prove ineffective against this bacterium. With the ability to trace the progression from neonatal infections to postinfectious hydrocephalus, the findings provide crucial insights for guiding diagnostics and interventions to prevent the devastating brain damage associated with this condition.
With confidence in the role of Paenibacillus bacteria as the cause of thousands of annual postinfectious hydrocephalus cases in Uganda, the team designated the condition as Neonatal Paenibacilliosis. They observed a geographical association with swampy regions near Lake Victoria and Lake Kyoga, where the Nile River’s during rainy seasons also correlated with increased cases, suggesting an environmental source for Paenibacillus.
Overcoming diagnostic limitations, the researchers employ geolocation and satellite rainfall data to predict Paenibacillus infection likelihood in newborns. Collaborating with local Ugandan hospitals, they strive to develop effective treatment protocols.
By investigating rural environments and cultural newborn care practices, they aim to pinpoint sources and implement preventive public health policies. Inspired by their success, the team extended their research to similar infections in Vietnam, Kenya, and the U.S.
Furthermore, they explore the possibility of low-cost sequencing systems for point-of-care diagnosis and personalized treatment. Driven by their dedication to improving child health, the researchers emphasize the collective efforts of doctors, scientists, and families in combating this critical issue and express gratitude for the opportunity to save newborn lives on a larger scale.
Journal Reference:
- Sarah U Morton, Christine Hehnly, et al., Paenibacillus spp infection among infants with postinfectious hydrocephalus in Uganda: an observational case-control study. The Lancet. DOI: 10.1016/S2666-5247(23)00106-4.
