Hip fractures are a common and serious injury, particularly among the elderly, often leading to significant healthcare costs and long-term consequences for the affected individuals. In the United Kingdom, the National Health Service (NHS) is vital in caring for patients with hip fractures, aiming to deliver high-quality and equitable healthcare services nationwide. However, recent research has revealed significant variations in health costs and care practices for hip fracture patients among different NHS hospitals and regions.
The University of Bristol, in collaboration with Versus Arthritis, conducted a study published in The Lancet Healthy Longevity on July 10th, emphasizing the need for evidence-based strategies to improve patient outcomes and reduce healthcare costs following hip fractures. With over 70,000 older adults admitted to UK hospitals annually due to hip fractures, the research analyzed data from 178,757 patients aged 60 and above in England and Wales between 2016 and 2019. Shockingly, the study found that more than one in four patients died within a year of their hip fracture. These findings highlight the urgency of addressing the challenges associated with hip fracture care in hospitals to enhance effectiveness and efficiency while improving patient outcomes.
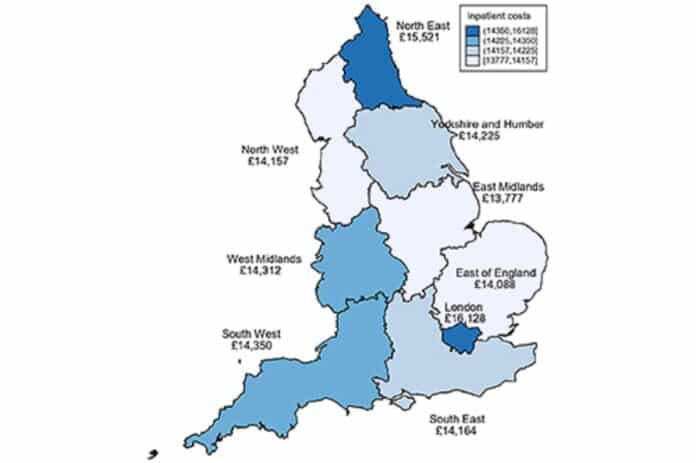
A study has revealed that patients experience an average hospital stay of 32 days following a hip fracture, resulting in significant inpatient costs averaging £14,642 per patient. These costs are comparable to those incurred the year after a stroke and surpass the costs associated with many common cancers. However, there were substantial variations in costs between hospitals, with a more than two-fold difference ranging from £10,867 to £23,188 per patient across 172 NHS hospitals in England and Wales.
The study also found that hospitals with early mobilization of patients after surgery and providing seven-day physiotherapy services had lower costs, and shorter hospital stays in the year following a hip fracture. Additionally, the research emphasized the vital role of orthogeriatricians and specialized geriatric consultants in providing adequate care for hip fracture patients.
According to Dr. Petra Baji, the first author of the study and a Senior Research Associate in Health Economics at Bristol Medical School: Translational Health Sciences (THS), assessing all hip fracture patients by an ortho geriatrician within the first few days of admission could lead to a cost reduction of £529 per patient and decrease the risk of death by 15% in the year following the fracture. Additionally, Dr. Rita Patel, a Senior Research Associate in Medical Statistics at Bristol, noted that if a consultant ortho geriatrician participates in hospital clinical governance meetings, an additional potential cost saving of £356 per patient could be achieved, along with reducing hospital days.
The study also found that hospitals with fracture liaison services had lower mortality rates and shorter hospital stays. These findings suggest that providing additional care through orthogeriatricians and fracture liaison services can improve efficiency in the NHS rather than increasing its burden.
The study underscores the importance of addressing the delivery of hip fracture care in hospitals to enhance effectiveness and efficiency while improving patient outcomes. The findings highlight the need for evidence-based quality improvement strategies across the UK to achieve financial savings while providing better care. Professor Celia Gregson, Chief Investigator of the study, emphasizes that the observed variations in patient outcomes and healthcare spending following hip fractures indicate room for improvement in the organization of care on a national scale.
Implementing measures such as prioritizing ortho geriatrician assessment, early mobilization after surgery, seven-day physiotherapy, delirium risk reduction, and regular multidisciplinary clinical governance meetings can improve patient outcomes and reduce healthcare spending in hospitals.
Caroline Aylott, Head of Research Delivery at Versus Arthritis, expressed concern about the state of care for older people who suffer hip fractures. The study revealed a high mortality rate within a year of the fracture and significant variations in the quality of care among NHS hospitals in England and Wales. Aylott emphasized the need for improved care for older individuals with multiple long-term conditions. The study also indicated that better access to orthogeriatricians and fracture liaison services could reduce mortality rates and improve recovery and cost savings for the NHS.
The research team has developed the REDUCE hip fracture service implementation toolkit in collaboration with the Royal Osteoporosis Society to support quality improvement in fracture services across 172 hospitals. The study was funded by Versus Arthritis and supported by the National Institute for Health and Care Research Bristol Biomedical Research Centre.
Caroline Aylott said, “The study found that better, faster access to orthogeriatricians and fracture liaison services would reduce people’s risk of dying, improve chances of better recovery, and reduce NHS spending. Just weeks after publication of the NHS workforce plan, the study provides further evidence of the desperate and immediate need for a properly resourced NHS.”
Journal Reference:
- Petra Baji, Rita Patel, et al., Organisational factors associated with hospital costs and patient mortality in the 365 days following hip fracture in England and Wales (REDUCE): a record-linkage cohort study. The Lancet.DOI:10.1016/S2666-7568(23)00086-7.