The new study in Stem Cell Reports pinpoints a drug target to seal leaks in small blood vessels, preventing cerebral small vessel disease. This condition is a significant factor in age-related cognitive decline. It is linked to nearly half of global dementia cases (45%). Additionally, it plays a role in one in five ischemic strokes, the standard type where a blood clot blocks blood and oxygen flow to the brain.
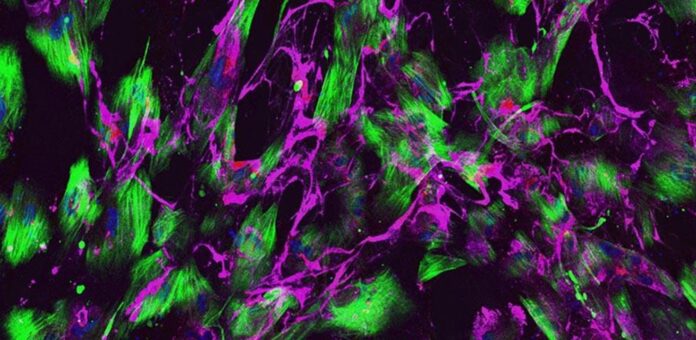
The majority of cases of SVD are linked to conditions like hypertension and type 2 diabetes, usually affecting people in their middle age. However, rare, inherited forms strike individuals in their mid-thirties. Scientists at the University of Cambridge used skin cells from patients with a rare genetic form of SVD caused by a COL4 gene mutation. By reprogramming these cells into induced pluripotent stem cells, they created a model mimicking the defects in brain vessels seen in patients.
Dr. Alessandra Granata from the Department of Clinical Neurosciences at Cambridge, who led the study, said: “Despite the number of people affected worldwide by small vessel disease, we have little in the way of treatments because we don’t fully understand what damages the blood vessels and causes the disease. Most of what we know about the underlying causes comes from animal studies, but they are limited in what they can tell us. That’s why we turned to stem cells to generate cells of the brain blood vessels and create a disease model ‘i’ a dish’ ‘hat mimics what we see in patients.”
Most cases of SVD are tied to conditions like hypertension, affecting middle-aged individuals. Yet, rare inherited forms can impact people in their mid-thirties. Scientists at the University of Cambridge used skin cells from those with a rare genetic form of SVD caused by a COL4 gene mutation. They created a model mimicking defects in brain vessels seen in patients by reprogramming these cells into induced pluripotent stem cells.
Dr. Granata added: “These drugs come with potentially significant side effects, so wouldn’t they be viable to treat small vessel disease? But they show that, in theory, targeting MMPs could stop the disease. Our model could be scaled up relatively easily to test the viability of future potential drugs.”
In conclusion, the study on lab-grown small blood vessels presents a promising avenue for treating a significant cause of stroke and vascular dementia. The findings deepen our understanding of the relationship between vessel damage and these health conditions and offer a potential drug target for future therapeutic interventions. This research represents a significant step toward developing innovative treatments for neurological disorders associated with small vessel disease.
Journal reference:
- Maha Al-Thani, Mary Goodwin-Trotman, et al., A novel human iPSC model of COL4A1/A2 small vessel disease unveils a key pathogenic role of matrix metalloproteinases. Stem Cells Reports. DOI: 10.1016/j.stemcr.2023.10.014.