Glioblastoma is a common, incurable brain tumor in adults. A recent study shows that a particular protein in the mitochondria plays a crucial role in Glioblastoma and could be a target for shrinking these tumors.
Brendan Harley (RBTE leader/EIRH), the Robert W. Schaefer Professor of Chemical and Biomolecular Engineering, said, “Glioblastoma is notorious for its lethality. One of the major challenges is that it spreads invasively throughout the brain. We’re interested in understanding what drives this process to identify new therapeutic strategies,”
In this study, researchers focused on a protein called CHCHD2 in the mitochondria. This protein’s name is complicated because it describes its structure like rope strands wound together.
The researchers checked a glioblastoma database called The Cancer Genome Atlas to see if they could find any links between CHCHD2 and cancer. They discovered that, out of 577 samples, the CHCHD2 genes were more active in tumor cells than in normal tissue, and their activity was even higher in advanced glioblastoma cases.
Rex Gaskins (RBTE), the Keith W. and Sara M. Kelley Endowed Professor of Immunophysiology in Animal Sciences and corresponding author of the study, said, “We also learned that in humans, the gene encoding CHCHD2 was closely linked to the gene encoding the epidermal growth factor receptor, or EGFR, on chromosome 7. A mutated version of this protein is found in over 50% of glioblastoma patients.”
When they saw that CHCHD2 was most active in patients with a mutation called EGFRvIII, the researchers understood that studying how these two proteins interact could be important for understanding glioblastoma.
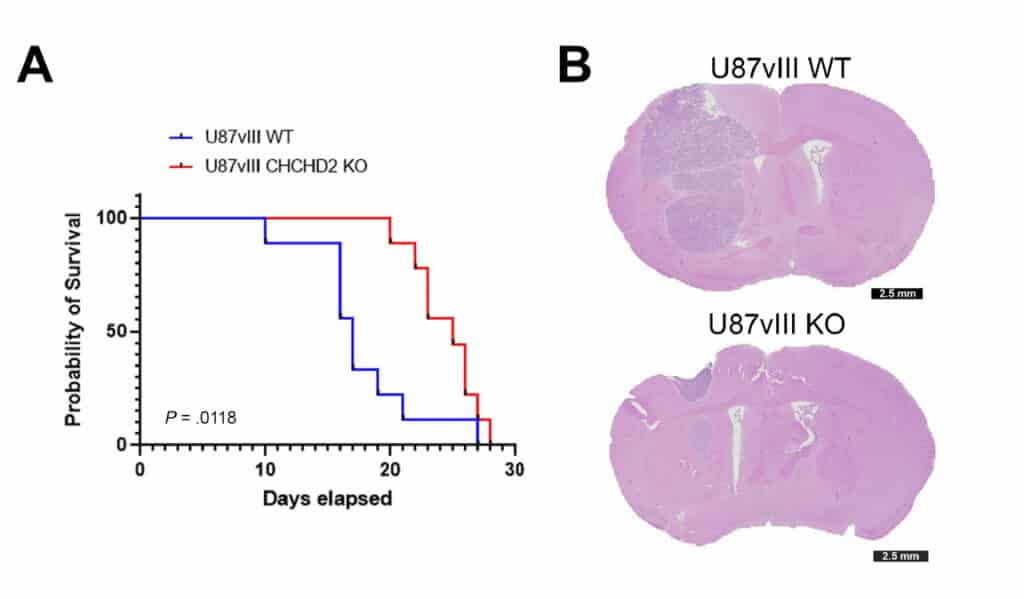
They tested CHCHD2’s impact on mouse tumor growth to check their idea. They compared mice with CHCHD2 and the mutated EGFR to mice without the mutated EGFR but without CHCHD2. The first group of mice survived for about 17 days, while the second group lived for 25 days. The mice that didn’t stay as long had more tumors spreading into the nearby brain tissue.
It’s clear that these proteins interact, but their role in glioblastoma progression still needs to be fully understood. The researchers have a few ideas based on their experiments.
First, they think CHCHD2 might make the mutated EGFR protein less responsive to drugs. Glioblastoma patients often don’t live very long, even with treatments like chemotherapy using temozolomide. The researchers found that cells with CHCHD2 and mutated EGFR were less affected by temozolomide than cells with just EGFR. This suggests that CHCHD2 could be a target for new treatments.
Another possibility is that CHCHD2 influences how EGFR promotes glioblastoma invasion. An experiment using a hydrogel to mimic the brain’s environment showed that cells with CHCHD2 and mutated EGFR were better at growing and spreading into the surrounding area. This was more noticeable when the oxygen level was low, which is common when glioblastoma cells spread from the tumor into the brain.
The data also provide evidence that CHCHD2 significantly impacts cellular metabolism, which was confirmed through various biochemical tests performed by the researchers. Gaskins said, “It’s a multifaceted paper that used patient data, human cell lines, and a mouse model of glioblastoma. All of our data are aligned, and we can pursue any of these mechanisms to see if it explains what is happening in the tumors.”
The researchers want to understand why these cells become more invasive, especially with little oxygen. They also plan to see if these findings apply to other types of glioblastomas that don’t have the same genetic mutation.
Harley, one of the researchers, said, “This study shows that CHCHD2’s role in glioblastoma was not fully recognized before, but it could be an important new target for improving treatment outcomes. It is valuable that this protein can change how cells act depending on their surroundings. We hope this discovery leads to new treatment ideas based on this key protein.”
In conclusion, this study shows that a protein in the mitochondria, called CHCHD2, is essential in how glioblastoma tumors develop and resist treatment. It can make the tumors less sensitive to chemotherapy, and it helps them spread into the brain. This discovery could lead to new therapies for glioblastoma, offering hope to patients who currently face limited options. Researchers are now looking into ways to target CHCHD2 to improve the outcomes for glioblastoma patients.
Journal reference:
- Jan C Lumibao, Payton L Haak et al., CHCHD2 mediates glioblastoma cell proliferation, mitochondrial metabolism, hypoxia‑induced invasion, and therapeutic resistance. International Journal of Oncology. DOI: 10.3892/ijo.2023.5565.
