Progress in understanding brain–viscera interoceptive signaling is hindered by a dearth of implantable devices suitable for probing brain and peripheral organ neurophysiology during behavior. Signals that regulate eating and other behaviors are constantly transmitted between the brain and the digestive system. This broad communication network affects our mental health and has been linked to various neurological illnesses.
MIT engineers have developed an innovative technique for examining those relationships. The researchers have demonstrated that they can manipulate the neural circuits in mice that connect the gut and the brain using fibers embedded with various sensors and light sources for optogenetic activation.
In a recent study, the researchers showed that affecting intestinal cells could make mice experience feelings of fullness or engage in reward-seeking behavior. They intend to investigate some of the connections between gut health and brain disorders, including autism and Parkinson’s disease, in subsequent research.
Polina Anikeeva, the Matoula S. Salapatas Professor in Materials Science and Engineering and a professor of brain and cognitive sciences, said, “The exciting thing here is that we now have technology that can drive gut function and behaviors such as feeding. More importantly, we can start accessing the crosstalk between the gut and the brain with the millisecond precision of optogenetics, and we can do it in behaving animals.”
“There’s continuous, bidirectional crosstalk between the body and the brain. For a long time, we thought the brain was a tyrant that sends output into the organs and controls everything. But now we know there’s a lot of feedback back into the brain, which potentially controls some of the functions we have previously attributed exclusively to the central neural control.”
Anikeeva set out to investigate the signals between the brain and the enteric nervous system, also known as the gut nervous system, as part of the center’s research. Through neural interaction and hormone release, gut sensory cells affect satiety and hunger.
Because there hasn’t been an effective means to quickly monitor the millisecond-long neuronal signals, separating those hormonal and neurological impacts has been challenging.
We needed a technology that didn’t exist to do gut optogenetics and then assess the effects on brain activity and behavior, which calls for millisecond accuracy. So we decided to create it.
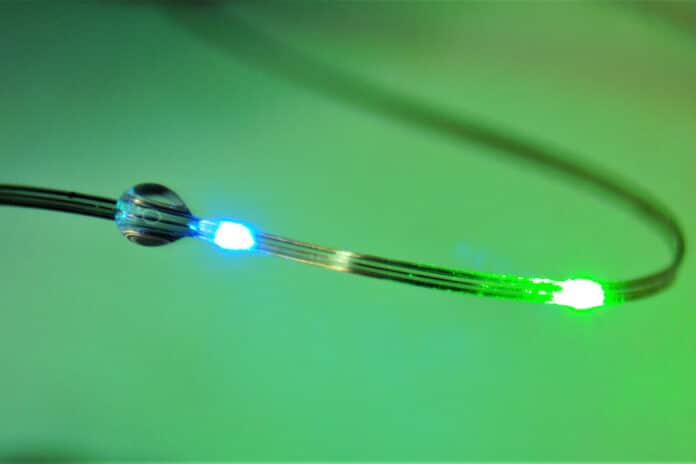
The flexible fibers used in the researchers’ electrical interface may perform several tasks and be implanted into the target organs. Using a method known as thermal drawing, researchers created polymer filaments that were about the same thickness as human hair and could be implanted with electrodes and temperature sensors.
Additionally, the filaments contain microfluidic channels that can be used to distribute medications and microscale light-emitting components that can stimulate cells optogenetically.
The fibers’ mechanical characteristics can be modified for various bodily parts. The scientists developed tougher, deeper-threading fibers specifically for the brain. They create more sensitive rubbery fibers for digestive organs like the gut that do not harm the organ lining but are yet strong enough to survive the harsh environment of the digestive tract.
Sahasrabudhe says, “To study the interaction between the brain and the body, it is necessary to develop technologies that can interface with organs of interest and the brain simultaneously while recording physiological signals with a high signal-to-noise ratio. We also need to selectively stimulate different cell types in both organs in mice so that we can test their behaviors and perform causal analyses of these circuits.”
Additionally, the fibers are made to be wirelessly controllable by a temporary attachment to the animal during an experiment using an external control circuit.
The researcher used this interface to conduct several studies demonstrating that they could affect behavior by altering the gut and the brain.
The ventral tegmental area (VTA), which releases dopamine, was the first area of the brain to receive optogenetic activation using the fibers. When the mice entered one of the three compartments of the cage, the researchers turned on the dopamine neurons in that chamber. The subsequent dopamine rush increased the likelihood of the mice returning to that chamber for the dopamine reward.
The researchers next looked to see if they might trigger such behavior by affecting the gut. To achieve this, scientists released sucrose using gut fibers, which also stimulated the production of dopamine in the brain and caused the animals to seek out the chamber in which the sucrose had been administered.
In collaboration with colleagues from Duke University, the researchers then discovered that omitting the sucrose and optogenetically stimulating gut nerve endings that send signals to the vagus nerve, which regulates digestion and other biological functions, could cause the same reward-seeking behavior.
Anikeeva says, “Again, we got this place preference behavior that people have previously seen with stimulation in the brain, but now we are not touching the brain. We are just stimulating the gut and observing control of central function from the periphery.”
Researchers next tested the fibers’ ability to control feeding behaviors. They discovered that the gadgets might optically trigger cells that make the hormone cholecystokinin, which encourages fullness. Even though the animals had been fasting for a while, their appetites were controlled when this hormone release was triggered. The same result was also seen when researchers stimulated cells to make PYY, a peptide that reduces hunger after consuming extremely rich foods.
The researchers now intend to use this interface to investigate neurological diseases that are thought to have a relationship between the gut and the brain. For instance, research has revealed that children with autism are far more likely than their peers to be diagnosed with GI dysfunction, and hereditary risks are associated with anxiety and irritable bowel syndrome.
Anikeeva says, “We can now begin asking, are those coincidences, or is there a connection between the gut and the brain? And there may be an opportunity for us to tap into those gut-brain circuits to begin managing some of those conditions by manipulating the peripheral circuits in a way that does not directly ‘touch’ the brain and is less invasive.“
Journal Reference:
- Sahasrabudhe, A., Rupprecht, L.E., Orguc, S. et al. Multifunctional microelectronic fibers enable wireless modulation of gut and brain neural circuits. Nature Biotechnology (2023). DOI: 10.1038/s41587-023-01833-5