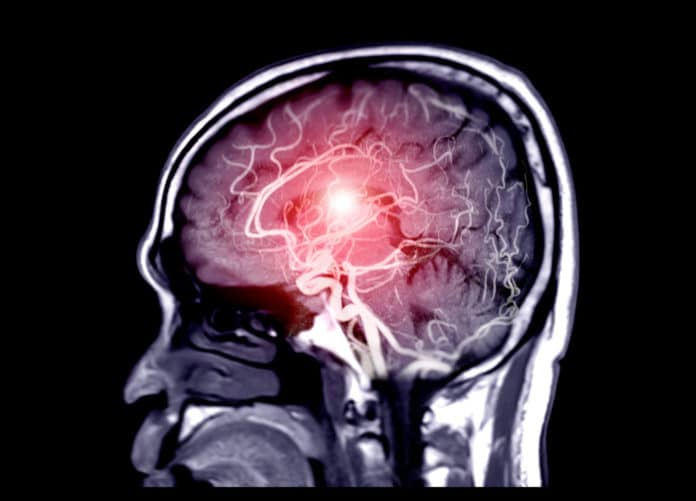
A new study that sheds light on how salt consumption affects brain health determined the connection between neuron activity and blood flow deep in the brain.
Neuron activation leads to a rapid increase in blood flow to the area. This relationship, known as neurovascular coupling, or functional hyperemia, occurs via dilation of blood vessels in the brain called arterioles.
Past studies on neurovascular coupling have been limited to superficial brain areas (such as the cerebral cortex). In these studies, scientists mainly focused on how sensory stimuli from the environment change the blood flow.
Little is known about whether the same principles apply to deeper brain regions attuned to stimuli produced by the body itself, known as interoceptive signals.
Scientists examined this relationship in brain regions using a newly developed approach that combines surgical techniques and state-of-the-art neuroimaging. They mainly focused on examing how the hypothalamus, a deep brain region involved in critical body functions including drinking, eating, body temperature regulation, and reproduction.
Scientists chose salt because the body needs to control sodium levels very precisely. Specific cells within our body detect how much salt is in your blood.
Dr. Javier Stern, professor of neuroscience at Georgia State and director of the university’s Center for Neuroinflammation and Cardiometabolic Diseases, said, “When you ingest salty food, the brain senses it and activates a series of compensatory mechanisms to bring sodium levels back down.”
“The body does this in part by activating neurons that trigger the release of vasopressin, an antidiuretic hormone that plays a key role in maintaining the proper concentration of salt.”
Unlike previous studies that found the connection between neuron activity and increased blood flow, scientists found a decrease in blood flow as the neurons activated in the hypothalamus.
Stern said, “The findings took us by surprise because we saw vasoconstriction, which is the opposite of what most people described in the cortex in response to a sensory stimulus. Reduced blood flow is normally observed in the cortex in the case of diseases like Alzheimer’s or after a stroke or ischemia.”
Scientists dubbed this phenomenon as ‘inverse neurovascular coupling’ or a decrease in blood flow that produces hypoxia. They also observed other differences: Vascular responses to stimuli are very localized in the cortex, and the dilation occurs rapidly. In the hypothalamus, the response was diffuse and took place slowly over a long period of time.
Stern said, “When we eat a lot of salt, our sodium levels stay elevated for a long time. We believe the hypoxia is a mechanism that strengthens the neurons’ ability to respond to the sustained salt stimulation, allowing them to remain active for a prolonged period.”
The study highlights essential questions such as how hypertension may affect the brain. It should be noted that between 50 and 60 percent of hypertension is believed to be salt-dependent.
Scientists are now planning to study this inverse neurovascular coupling mechanism in animal models to determine whether it contributes to the pathology of salt-dependent hypertension.
This new study is expected to study other brain regions and diseases, including depression, obesity, and neurodegenerative conditions.
Stern said, “If you chronically ingest a lot of salt, you’ll have hyperactivation of vasopressin neurons. This mechanism can then induce excessive hypoxia, which could lead to tissue damage in the brain. If we can better understand this process, we can devise novel targets to stop this hypoxia-dependent activation and perhaps improve the outcomes of people with salt-dependent high blood pressure.”
Journal Reference:
- Ranjan K. Roy et al. Inverse neurovascular coupling contributes to positive feedback excitation of vasopressin neurons during a systemic homeostatic challenge. DOI: 10.1016/j.celrep.2021.109925