In recent breakthroughs in cancer immunotherapy, a combination of biomaterials has been employed to enhance treatment efficacy. By delivering a powerful one-two punch, these biomaterials augment the body’s immune response against cancer cells, improving therapeutic outcomes.
This innovative approach holds promising potential for revolutionizing cancer treatment and providing new avenues for patients to combat the disease. In this article, we explore the concept of biomaterial-delivered cancer immunotherapy and its significant impact on advancing the field of oncology.
The success of cancer immunotherapy, particularly adoptive T cell, and immune checkpoint inhibitor therapies, has significantly improved patient outcomes in terms of survival and quality of life. However, these therapies have shown limited effectiveness in treating solid tumors, which account for approximately 90% of all tumors.
This is primarily due to various challenging barriers. Adoptive T cell therapies involve engineering a patient’s T cells outside the body to recognize and destroy tumor cells by binding to specific surface features (antigens).
However, once reintroduced into the patient’s bloodstream, these engineered T cells face obstacles such as traveling long distances to reach the solid tumor, limited infiltration into the tumor mass, suppression of their cytotoxic activity by tumor cells and the surrounding microenvironment, and the ability of solid tumors to develop heterogeneity in their cell composition and evade the attack of adoptively transferred T cells.
Overcoming these barriers is crucial for enhancing the efficacy of adoptive T-cell therapies in treating solid tumors.
A team of immune engineers from the Wyss Institute for Biologically Inspired Engineering at Harvard University and Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) has introduced a groundbreaking immunotherapy approach called SIVET (synergistic in situ vaccination enhanced T cell).
This innovative technique utilizes a biomaterial-based injectable system to address the barriers encountered in adoptive T-cell therapies for solid tumors.
SIVET facilitates localized delivery of antigen-specific T cells directly to tumor sites, ensuring prolonged activation and broader immune system engagement. In preclinical studies involving mice with melanomas, an aggressive form of solid tumor, SIVET demonstrated rapid tumor regression and long-term protection against tumor recurrence.
The research findings, published in Nature Communications, highlight the potential of SIVET in revolutionizing cancer immunotherapy.
Senior author David Mooney, Ph.D., who is a Founding Core Faculty member at the Wyss Institute and the Robert P. Pinkas Family Professor of Bioengineering at SEAS, said, “In the SIVET approach, we essentially combined fast-acting adoptive T cell therapy with long-term protective cancer vaccine technology in a locally delivered integrated biomaterial. Advancing this approach towards patient settings could help addresses several limitations of current immunotherapies and offers new inroads into the treatment of solid tumors.”
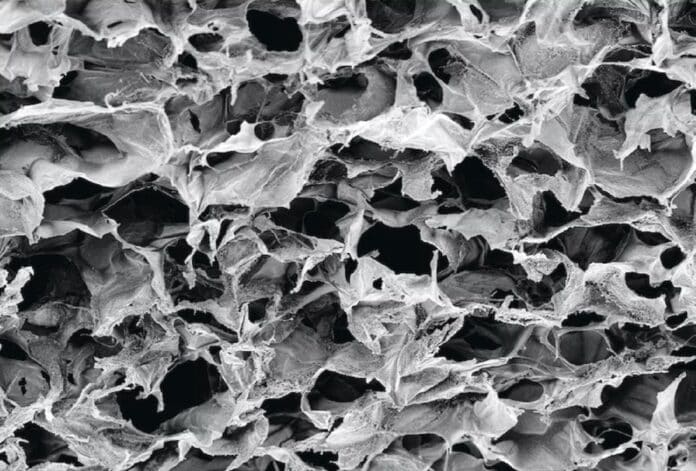
Researchers led by Dr. David Mooney from the Wyss Institute at Harvard University have developed a biomaterial-based immunotherapy approach that combines adoptive T-cell therapy with cancer vaccines. The team designed a cryogel biomaterial containing collagen and alginate polymers that act as a 3D porous scaffold.
This biomaterial is injected near the tumor site. It gradually releases interleukin 2 (IL2), a cytokine that supports the expansion of the delivered T cells. The T cells move out of the biomaterial and attack the tumor cells. This novel approach aims to quickly reduce tumor size while engaging the immune system deeper, offering potential improvements in cancer treatment.
The SIVET (synergistic in situ vaccination enhanced T cell) approach, developed by researchers at the Wyss Institute at Harvard University, combines adoptive T cell therapy with a biomaterial-based cancer vaccine.
The biomaterial releases cytokines, including interleukin 2 (IL2) and GMCSF, attracting and activating host antigen-presenting cells (APCs) near the tumor site. The APCs infiltrate the tumor, capture new antigens from dying tumor cells, and migrate to nearby lymph nodes to trigger a broader immune response.
In a mouse melanoma model, SIVET demonstrated superior tumor control compared to direct injection of T cells into the tumor or infusion into the bloodstream. SIVETs prolonged the activity of delivered T cells and prevented the exhaustion of all T cells in the tumor microenvironment.
The biomaterial’s vaccine component trained the immune system to reject melanoma tumors for extended periods, improving survival. The study highlights the potential of this transdisciplinary approach to enhance immunotherapeutic strategies against solid cancers.
Journal Reference:
- Adu-Berchie, K., Brockman, J.M., Liu, Y. et al. Adoptive T cell transfer and host antigen-presenting cell recruitment with cryogel scaffolds promote long-term protection against solid tumors. Nature Communications. DOI:10.1038/s41467-023-39330-7.