An affordable way to quantify childhood and teenage obesity that may eventually take the place of body mass index (BMI) is the waist circumference-to-height ratio, according to a recent study. Compared to BMI, this measure was more accurate in identifying extra fat mass and differentiating it from muscle mass in children and adolescents.
The study, conducted by collaboration between University of Bristol, University of Exeter in the UK and University of Eastern Finland, was published in Pediatric Research.
Obesity in childhood and adolescence is pervasive, impacting about one in four children today. It’s a severe concern since it can result in adult health issues, including diabetes, heart disease, and even early death. Accurately identifying childhood obesity is crucial for timely intervention.
For a long time, the BMI (body mass index) and weight-to-height charts have been used to determine whether a child is obese. However, these techniques must be improved since they cannot distinguish between muscle and fat. Therefore, two children may not have the same amount of fat while having the same BMI.
Expensive tools like the DEXA scan can accurately measure fat and muscle, but they’re challenging to find in regular healthcare centers. The American Academy of Pediatrics has asked for cheaper, more accurate ways to measure obesity.
According to specific adult research, waist circumference measures, as opposed to height, are a more accurate indicator of early mortality than BMI. However, the appropriate assessment and how well this approach works in children and adolescents need to be clarified. This investigation seeks to learn.
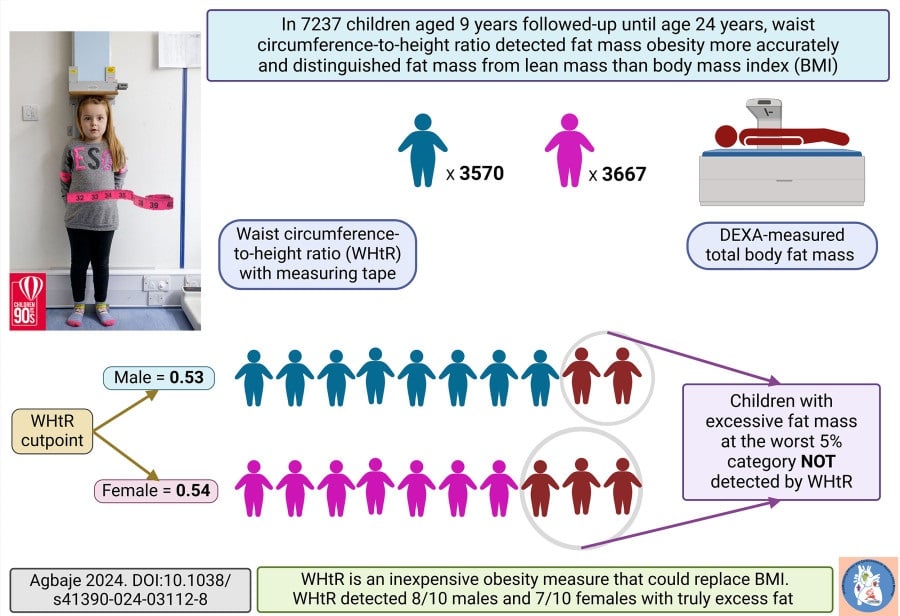
Using data from the University of Bristol’s Children of the 90s project, this study followed 7,237 kids from age 9 to 24, measuring their BMI and waist circumference-to-height ratio at different times. It’s the most extensive and most extended study of its kind worldwide.
The waist circumference to height ratio matched DEXA scans quite well (81–89%) for fat mass but not as well (24–39%) for muscle mass. BMI and muscle mass (52–58%) and fat mass (65-72%) agreed well. It’s difficult to determine if BMI counts muscle or excess fat. The optimal waist-to-height ratios for predicting extra fat were also determined.
Andrew Agbaje, an award-winning physician and pediatric clinical epidemiologist at the University of Eastern Finland, said, “This study provides novel information that would be useful in updating future childhood obesity guidelines and policy statements. The average waist circumference-to-height ratio in childhood, adolescence, and young adulthood is 0.45; it does not vary with age and among individuals like BMI.”
“Waist circumference-to-height ratio might be preferable to BMI assessment in children and adolescent clinics as an inexpensive tool for detecting excess fat. Parents should not be discouraged by their children’s BMI or weight but can inexpensively confirm whether the weight is due to increased excess fat by examining their kid’s waist circumference-to-height ratio.” He added.
The waist-to-height ratio is better than BMI at spotting fat obesity in kids and teens. More research is needed to confirm this and understand how it can help doctors better assess obesity in children.
Journal reference:
- Agbaje, A.O. Waist-circumference-to-height-ratio had a better longitudinal agreement with DEXA-measured fat mass than BMI in 7237 children. Pediatric Research. DOI: 10.1038/s41390-024-03112-8.
