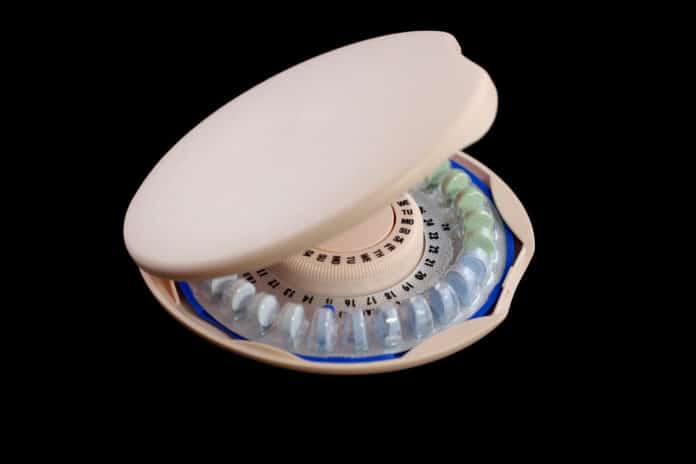
Since the beginnings of civilization, people have used contraception to prevent pregnancy. Access to effective contraceptives is key to women’s well-being and autonomy – family planning reduces women’s health risks, decreases infant mortality, reduces the incidence of abortion, and slows population growth.
Birth control, in simple words, is how women prevent pregnancy. There are lots of different birth control options out there. But, with the exception of abstinence, no method of birth control is perfect. Half of all unintended pregnancies occur while a couple is using birth control.
What leads to birth control failure?
Besides human error, there are other potential reasons a particular method of birth control might fail. Now, in a new study by the University of Colorado Anschutz Medical Campus, scientists have offered a clue on why some women get pregnant while using birth control.
Scientists have found that women who get pregnant while using birth control may carry a gene that breaks down the hormones common in contraceptives.
For the study, scientists looked at 350 healthy women with a median age of 22.5 years old and a contraceptive implant in place for between 12 and 36 months. Almost 5 percent of women tested had a gene called CYP3A7*1C that is usually active in fetuses and then switched off before birth. But some women with this gene continue to make the CYP3A7 enzyme into adulthood.
Study’s lead author Aaron Lazorwitz said, “That enzyme breaks down the hormones in birth control and may put women at a higher risk of pregnancy while using contraceptives, especially lower dose methods. The variant could be found during genetic screening.”
“When a woman says she got pregnant while on birth control, the assumption was always that it was somehow her fault. But these findings show that we should listen to our patients and consider if there is something in their genes that caused this.”
The study also highlights how pharmacogenomics, a relatively new field that analyzes how genes affect a person’s response to drugs, has the potential to alter the field of women’s health dramatically.
Lazorwitz said, “The study may help spur the development of more precise medical tools that can help tailor treatment to individual patients. As more genetic data become available, clinicians may need to consider adding genetic predisposition to increased steroid hormone metabolism in their differential diagnosis for unintended pregnancies in women reporting perfect adherence to hormonal contraceptive methods.”
The study co-authors include Christina L. Aquilante, PharmD; Kris Oreschak, BS; Jeanelle Sheeder, Ph.D.; Maryam Guiahi, MD, MSc; Stephanie Teal, MD, MPH.
Journal Reference:
- Aaron Lazorwitz, Christina L. Aquilante, Kris Oreschak, Jeanelle Sheeder, Maryam Guiahi, Stephanie Teal. Influence of Genetic Variants on Steady-State Etonogestrel Concentrations Among Contraceptive Implant Users. Obstetrics & Gynecology, March 11, 2019; DOI: 10.1097/AOG.0000000000003189