Metastasis is the spread of cancer cells to new areas of the body, often through the lymph system or bloodstream. Some kinds of cancer are more likely to spread to the lung than others. This is known as lung metastases.
Currently, there are not any approved treatment available for lung metastasis. As a solution, scientists at Harvard’s Wyss Institute for Biologically Inspired Engineering and John A. Paulson School for Engineering and Applied Sciences (SEAS) have developed a technique that may turn this grim prognosis into less grim.
Scientists focused on treating the metastasis itself by delivering immune-cell-attracting chemicals into lung cancers via red blood cells. In experiments with mice, the approach stops tumor growth with metastatic breast cancer. Also, it acted as a vaccine and protected the animals against future cancer recurrences.
Co-first author Zongmin Zhao, a postdoctoral fellow at the Wyss Institute and SEAS, said, “Our approach is the exact opposite of conventional cancer treatments that focus on getting the immune system to recognize and attack the primary tumor because those tumors are often large and difficult for immune cells to penetrate. We recognized that the high density of blood vessels in the lungs provides much better access to tumors there, offering a unique opportunity to induce an immune response by targeting the metastasis.”
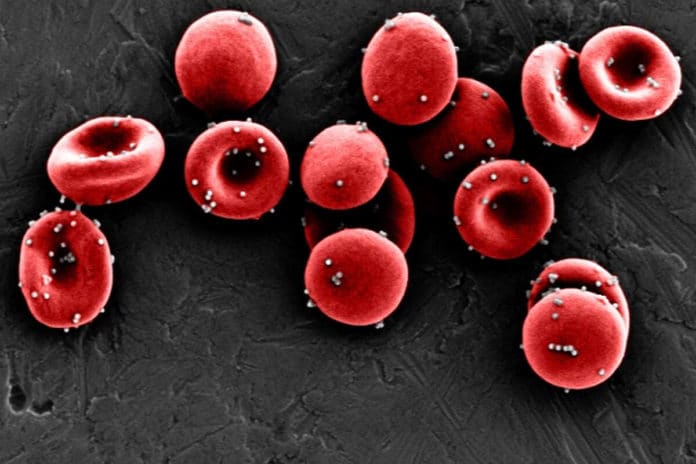
Recently, scientists have discovered that attaching drug-filled nanoparticles to red blood cells allows them to escape detection and stay in the body long enough to deliver their payloads while minimizing toxicity.
Scientists decided to use the same technique to determine if they could deliver immune-system-stimulating chemicals to metastatic lung tumors rather than chemotherapy, damaging lung tissue. They chose a chemokine, a small protein that attracts white blood cells, called CXCL10 as their payload.
When cancer goes through metastasis, the branching blood vessels that allow oxygen to diffuse from the lungs’ air sacs into red blood cells are small to such an extent that a rogue cancer cell circulating in the bloodstream can quickly get stuck there and take up residence, ultimately developing into a secondary tumor. When set up, metastatic tumors release a campaign of chemical cues that ruin the body’s defenses, hampering endeavors to induce an immune response.
Co-first author Anvay Ukidve, a graduate research fellow at the Wyss Institute and SEAS who is now a scientist at a pharmaceutical company, said, “Lung metastases deplete certain kinds of chemokines from their local environment, which means the signal that should attract healthy white blood cells to fight the tumor is gone. We hypothesized that providing that chemokine signal at the tumor site could help restore the body’s normal immune response and enable it to attack the tumors.”
At first, scientists optimized their nanoparticles to ensure that they would detach from their red blood cell hosts only when the blood cells made their tight squeeze through the lungs’ tiny capillaries. They also decorated the nanoparticles’ surfaces with an antibody that attaches to a protein commonly found on lung blood vessel cells called ICAM-1 to increase the nanoparticles’ retention in the lungs.
These nanoparticles were then filled with the chemokine CXCL10, creating a package the researchers named ImmunoBait. ImmunoBait particles were then attached to mouse red blood cells to develop a therapeutic delivery system named erythrocyte-anchored systemic immunotherapy (EASI) and injected into the bloodstreams of mice with breast cancer that had metastasized to their lungs.
ImmunoBait particles stayed in the animals’ lungs for up to six hours after EASI injection, and most of them were distributed in and around the metastases. Treatment with EASI led to strong expression of CXCL10 for up to 72 hours, suggesting that delivering the chemokine stimulated the body to start producing it on its own, despite the immunosuppressive tumor microenvironment.
To find out exactly what effect the delivered CXCL10 had on the mice’s immune systems, the team analyzed the different types of cells present in the lungs before and after EASI injection. They observed increases in the infiltration of T helper type 1 (Th1) CD4 cells, which release pro-inflammatory chemicals that help keep tumors under control and effector CD8 cells and natural killer (NK) cells, which drive the direct killing of cancer cells.
Armed with proof that their system could attract immune cells to lung metastases, the team then tested its ability to slow or halt the disease’s progression in mice. They first removed the animal’s breast cancer tumors, then injected them with either CXCL10 alone, ImmunoBait nanoparticles alone, or EASI.
EASI inhibited lung metastasis progression with four-fold and six-fold greater efficacy than free CXCL10 and ImmunoBait, respectively. All of the EASI-treated mice had fewer than 20 metastatic nodules after 37 days, and 25 percent of them had only one nodule.
In contrast, mice that received the other therapies had anywhere from two to 100 nodules. The mice that received EASI also had nearly three-fold better survival. While animals in all the different treatment groups succumbed to their disease in less than 20 days, about 25 percent of the EASI-treated mice survived 40 days. They were also free of any signs of off-target toxicity or other adverse effects from the treatment.
Because EASI effectively activated the immune system against lung metastases, the researchers wondered if that activation could provide lasting protection against future recurrences of same cancer. They analyzed the blood of mice that had received EASI and observed an increased number of memory CD8 cells, which persist long-term after an immune threat and sound the alarm if that threat resurfaces.
To test whether those memory cells provided sufficient protection, the team re-inoculated mice with the same tumor cells two days after their last treatment. Mice treated with EASI had significantly slower tumor growth, and tumor weight than mice injected with saline or left untreated, demonstrating that local treatment of lung metastases produced systemic immunity against tumor development.
Senior author Mitragotri, who is also a Hiller Professor of Bioengineering and the Hansjörg Wyss Professor of Biologically Inspired Engineering at SEAS, said, “These findings highlight the ability of our EASI system to convert the biological adversity of metastasis into a unique therapeutic opportunity against metastatic cancers.”
Journal Reference:
- Zhao, Z., Ukidve, A., Krishnan, V. et al. Systemic tumor suppression via the preferential accumulation of erythrocyte-anchored chemokine-encapsulating nanoparticles in lung metastases. Nat Biomed Eng (2020). DOI: 10.1038/s41551-020-00644-2