Peanuts are one of the most common food allergens for children. Most severe cases lead to a potentially deadly immune reaction called anaphylactic shock. Currently, only one approved treatment reduces the severity of the allergic reaction, and it takes months to kick in.
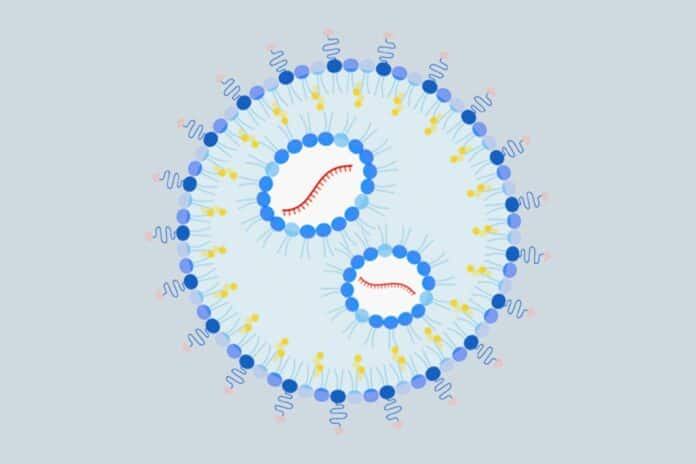
A group of UCLA immunologists has devised a first-of-its-kind mRNA treatment that could wipe out a peanut allergy. They developed a first-of-its-kind nanoparticle that delivers mRNA to particular liver cells by drawing inspiration from COVID-19 vaccinations and their studies into the illness. These cells then instruct the body’s defensive mechanisms to accept peanut proteins.
When tested on mice, the nanoparticle not only reversed peanut allergies but also prevented them from developing.
Dr. André Nel, the paper’s co-corresponding author, a UCLA distinguished professor of medicine and director of research at the California NanoSystems Institute at UCLA, said, “As far as we can find, mRNA has never been used for allergic disease. We’ve shown that our platform can work to calm peanut allergies, and we believe it may do the same for other allergens, in food and drugs, as well as autoimmune conditions.”
Scientists mainly focused on the liver. There are two reasons behind it: First, the organ doesn’t respond to every challenge because it is regularly bombarded with foreign substances, including allergens. Second, the organ is home to antigen-presenting cells, which collect foreign proteins and train the immune system to tolerate them rather than attack when they’re detected.
The investigation extends to two earlier discoveries. They discovered in 2021 that a nanoparticle that delivered a specifically chosen protein fragment, known as an epitope, to the liver reduced the symptoms of deadly egg allergy in mice. The next year, they discovered one epitope that, when given to mice’s livers via a nanoparticle, reduced their sensitivity to peanuts. These epitopes are anticipated to be safer as a component of treatment because they omit the portion of the peanut or egg protein that causes allergies.
Dr. Nel said, “If you’re lucky enough to choose the correct epitope, there’s an immune mechanism that puts a damper on reactions to all of the other fragments. That way, you could care for a whole ensemble of epitopes that play a role in disease.”
By including a sugar molecule on the surface of their earlier nanoparticle that binds selectively to cells that present antigens, the scientists improved upon its design. Another development was the use of mRNA.
As with mRNA vaccines for SARS-CoV-2, the scientists engineered a portion of the mRNA payload in the upgraded nanoparticle to encode the chosen epitope or epitopes, in this case, the peanut protein fragment found in a prior investigation. Utilizing mRNA makes loading the nanoparticle simpler and removes the difficulties associated with incorporating more than one epitope, a benefit that could broaden the use. For instance, numerous epitopes may be required to treat specific other allergies or multiple allergies.
The researchers administered their improved nanoparticle to six mice in two doses, separated by a week, to test whether it would prevent peanut allergies. Another set of six mice received a nanoparticle with the same mRNA payload but without any targeting sugar on its surface. Six other mice received the updated nanoparticle but with mRNA inside that did not code for any protein or epitope.
A third group of six mice received no nanoparticles at all. To make the mice more sensitive to the peanut allergens, scientists began giving the mice a crude peanut protein extract one week following the second treatment. They subjected the mice to peanut protein for another week to cause anaphylactic shock.
While more severe symptoms manifested in the control group receiving no treatment and the group receiving a targeted nanoparticle with noncoding mRNA, mice pretreated with the improved nanoparticle displayed lower symptoms than mice who received a nanoparticle without targeting sugar.
The experiment was repeated, but this time the steps were carried out in a different order, exposing the mice to peanut protein before administering the nanoparticle. Once more, the improved nanoparticle functioned better than a comparable one without the targeting sugar, and both produced noticeably fewer side effects in mice than what the researchers saw in mice who received either no treatment or a nanoparticle with noncoding mRNA.
Scientists examined the quantities of particular immune cells, antibodies, enzymes, and cytokines in both experiment iterations to confirm that the enhanced nanoparticle had improved the animals’ tolerance for peanut protein.
Nel predicts that if additional lab tests are successful, the nanoparticle might begin clinical trials in three years. The regulatory process necessary to test the strategy for peanut allergies in clinical trials will shortly be started in his lab. He went on to say that by changing the mRNA payload to one that codes for different epitopes, it is possible to modify the nanoparticle to treat other autoimmune diseases and allergies.
Scientists are now exploring whether the nanoparticle could be used to treat type 1 diabetes, a disease in which the immune system attacks cells in the pancreas that enable the body to get energy from food. Important epitopes from the proteins that trigger the immune attack in diabetes have already been identified by other researchers.
Journal Reference:
- Xiao Xu, Xiang Wang et al. Use of a Liver-Targeting Immune-Tolerogenic mRNA Lipid Nanoparticle Platform to Treat Peanut-Induced Anaphylaxis by Single- and Multiple-Epitope Nucleotide Sequence Delivery. ACS Nano. DOI: 10.1021/acsnano.2c12420