Childhood obesity is a severe problem in the United States, putting children and adolescents at risk for poor health. The percentage of children affected by obesity has more than tripled since the 1970s.
A recent study suggests that obesity triggers inflammation in the nervous system that could damage essential regions of the brain. Scientists used MRI and found damage that may be related to inflammation in the minds of obese adolescents.
Developments in MRI like diffusion tensor imaging (DTI), a technique that tracks the diffusion of water along the brain’s signal-carrying white matter tracts, have enabled scientists to study this damage directly.
During the study, scientists compared DTI results in 59 obese adolescents and 61 healthy adolescents, ages 12 to 16 years. From DTI, the researchers derived a measure called fractional anisotropy (FA), which correlates with the condition of the brain’s white matter. A reduction in FA is indicative of increasing damage in the white matter.
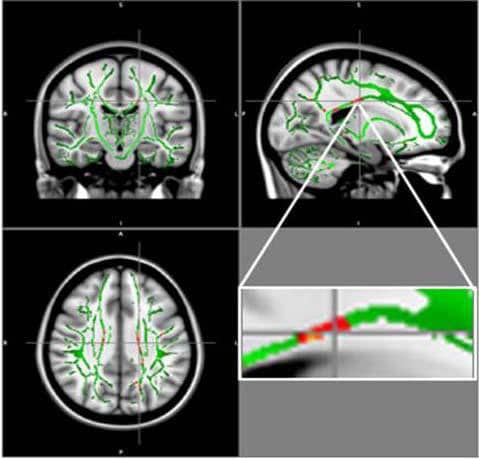
The outcomes demonstrated a decrease of FA values in the obese teenagers in regions situated in the corpus callosum, a bundle of nerve fibers that connects the left and right hemispheres of the brain. A decrease of FA was likewise found in the middle orbitofrontal gyrus, a brain region related to emotional control and the reward circuit. None of the brain areas in obese patients had increased FA.
Such kind of damage pattern correlated with some inflammatory markers like leptin, a hormone made by fat cells that helps regulate energy levels and fat stores. In some obese people, the brain does not respond to leptin, causing them to keep eating despite adequate or excessive fat stores. This condition, known as leptin resistance, makes the fat cells produce even more leptin.
The worsening condition of the white matter was also associated with levels of insulin, a hormone produced in the pancreas that helps regulate blood sugar levels. Obese people often suffer from insulin resistance, a state in which the body is resistant to the effects of the hormone.
Co-author Pamela Bertolazzi, a biomedical scientist and Ph.D. student from the University of São Paulo in Brazil, said, “Brain changes found in obese adolescents related to important regions responsible for the control of appetite, emotions and cognitive functions.”
Dr. Bertolazzi said, “Our maps showed a positive correlation between brain changes and hormones such as leptin and insulin. Furthermore, we found a positive association with inflammatory markers, which leads us to believe in the process of neuroinflammation besides insulin and leptin resistance.”
“Additional studies are needed to determine if this inflammation in young people with obesity is a consequence of the structural changes in the brain.”
“In the future, we would like to repeat brain MRI in these adolescents after multi-professional treatment for weight loss to assess if the brain changes are reversible or not.”
The study being presented next week at the annual meeting of the Radiological Society of North America (RSNA).
