It is becoming more apparent how lipids function in both physiological and pathological aspects of human metabolism, especially in type 2 diabetes. Scientists can now measure the amounts of several hundred distinct types of lipids simultaneously, each having unique properties and impacts on human metabolism that can be either beneficial or harmful. This is made possible by state-of-the-art techniques, one of which is mass spectrometry.
The most prevalent lipids in type 2 diabetics may be identified, which could serve as a foundation for various treatments. These could include early detection, prevention, identification of possible therapeutic targets, or individualized advice. For this reason, researchers at Geneva University Hospitals (HUG) and the University of Geneva (UNIGE) thoroughly examined the blood profiles of patients enrolled from four different European nations.
Scientists made two significant discoveries. By analyzing the blood profiles of dozens of people suffering from diabetes or pre-diabetes or who have had their pancreas partially removed, they found:
- The lipid composition of blood and adipose tissues varies during the day and changes depending on the time of day in people with diabetes, who have more significant amounts of toxic lipids.
- Furthermore, in situations where the beta cells that ordinarily secrete insulin are unable to do so, lysoPI, a particular form of lipid, can help with insulin secretion.
Scientists, in particular, conducted a “lipidomic” analysis of two groups of patients. They wanted to establish the profile, over a 24-hour cycle, of multiple lipids present in the blood and adipose tissues.
The lipid profiles of individuals with type 2 diabetes and those without the disease differ more in the early morning when specific harmful lipids are more prevalent. The reason behind this still needs to be discovered. However, this could indicate the severity of diabetes and pave the way for personalized care according to each patient’s specific chronotype.
The implications extend beyond diabetes: results may be skewed and contradict one another if samples are collected at drastically different times of the day.
This study not only involved people but also a mouse model of pre-diabetes and patients who had lost around half their insulin-producing beta cells after surgery.
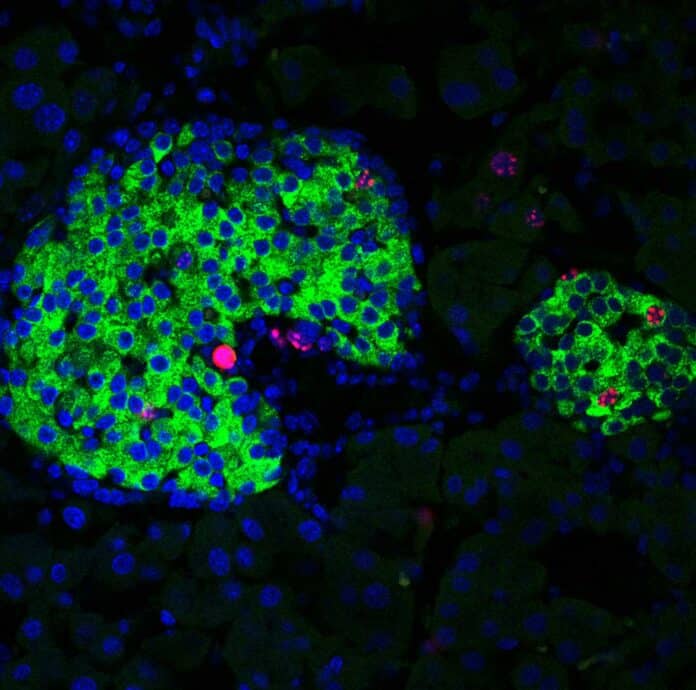
They discovered that a type of lipid, lysoPIs, increases when there is a sharp decrease in functional β cells, even before the onset of clinical symptoms of diabetes.
The scientists then administered lysoPI to diabetic mice and observed increased insulin production.
Pierre Maechler, a professor in the Department of Cell Physiology and Metabolism at the UNIGE Faculty of Medicine and members of the Diabetes Faculty Centre, said, “The same phenomenon occurred in vitro, on pancreatic cells from diabetic patients. The lysoPIs can reinforce insulin secretion by acting as a crutch when the number of beta cells decreases or when these cells malfunction. Yet, certain foods, such as legumes, naturally contain lysoPI precursors.”
Scientists can investigate hitherto uncharted territory by shedding light on the previously unknown function of lysoPIs. One intriguing approach to managing diabetes may be the creation of lysoPI receptor-specific compounds or dietary supplements and a more thorough consideration of patients’ chronobiological profiles. Diabetes is a complicated illness that requires far more individualized care than is provided at the moment.
Journal References:
- Flore Sinturel, Simona Chera et al. Circadian organization of lipid landscape is perturbed in type 2 diabetic patients. Cell Reports Medicine. DOI: 10.1016/j.xcrm.2023.101299
- Cecilia Jiménez-Sánchez; Flore Sinturel; Teresa Mezza et al. Lysophosphotidylinositols (LysoPIs) are upregulated following human ß-cell loss and act to potentiate insulin release. Diabetes. DOI: 10.2337/db23-0205