COVID-19 symptoms can sometimes persist for months. Even those who had mild versions of the disease, some people continue to experience symptoms after their initial recovery.
Such people are referred to as long haulers, and the conditions have been called post-COVID-19 syndrome or long COVID-19.
COVID-19 long-haulers at increased likelihood of developing kidney damage and chronic and end-stage kidney diseases, suggests a new study at Washington University School of Medicine in St. Louis and the Veterans Affairs St. Louis Health Care System.
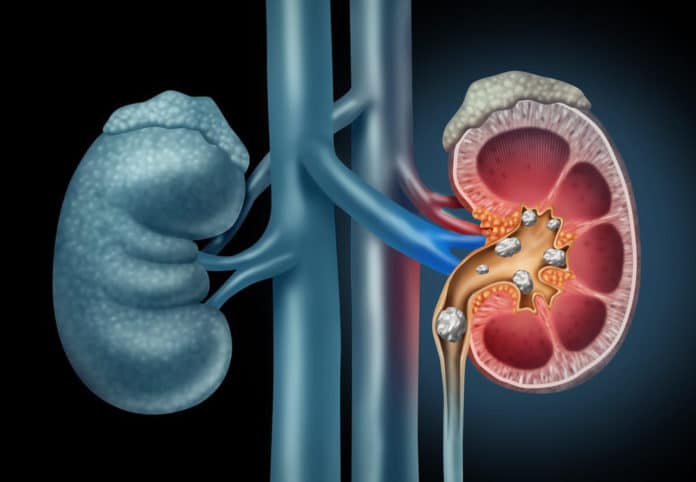
Kidney disease, also referred to as a silent killer, affects 37 million people in the U.S. and is one of the nation’s leading causes of death.
This study highlights the importance of paying attention to kidney function and disease in caring for patients who have had COVID-19.
Compared with patients who did not become infected, COVID-19 long haulers had a 15% higher risk of suffering from a significant adverse kidney event such as chronic kidney disease, a 30% higher risk of developing acute kidney injury, and a 215% higher risk of acquiring end-stage kidney disease.
Senior author Ziyad Al-Aly, MD, an assistant professor of medicine at Washington University, said, “If kidney care isn’t an integral part of COVID-19 post-acute care strategy, then we will miss opportunities to help potentially hundreds of thousands of people who have no idea that their kidney function has declined due to this virus. This is in addition to the millions of Americans who suffer from kidney disease not caused by COVID-19.”
“Based on our research, we believe that 510,000 of those people who have had COVID-19 may have kidney injury or disease.”
Scientists analyzed de-identified medical records in a database maintained by the U.S. Department of Veterans Affairs, the nation’s largest integrated healthcare delivery system. They created a controlled dataset that included more than 1.7 million healthy and COVID-infected veterans from March 1, 2020, through March 15, 2021. Of those veterans, 89,216 had confirmed COVID-19 diagnoses and made it through the acute phase.
Most of the patients in the study were men in their late 60s. Scientists also analyzed 151,289 women, including 8,817 with COVID-19, and adults of all ages.
Among the COVID-19 patients, 12,376 (13.9%) required hospitalization, including 4,146 (4.6%) who were admitted to intensive care units (ICUs).
Al-Aly said, “The risk of decreased kidney function is highest among people who were in the ICU; however, it’s important to note that the risk extends to all patients, even those who had milder cases of COVID-19.”
“It’s essential to discover kidney dysfunction before the problem progresses and becomes harder to treat. But kidney problems are silent problems that won’t be found until somebody checks the bloodwork. Based on our research, it’s essential that healthcare providers do this for people who have had COVID-19. Otherwise, we’ll miss a lot of people and, sadly, we’ll be dealing with more advanced kidney diseases down the road.”
“People who were hospitalized for COVID-19 or needed ICU care are at the highest risk. But the risk is not zero for those who had milder cases. It’s significant. And we need to remember that we don’t yet know the health implications for long-haulers in the coming years.”
After the underlying 30 days of COVID-19 contamination, 4,757 (5.3%) of the patients experienced a reduction of 30% or more in glomerular filtration rates (GFR), which doctors use to assess kidney function and, if relevant, decide the severity of kidney disease. A simple blood test determines the severity rate.
Scientists found that people with milder COVID-19 cases had 1.09 times the risk of an estimated GFR decline of 30% or more. For hospitalized COVID-19 patients not in intensive care units, there was two times the risk of having an estimated GFR decrease of 30% or more. In comparison, intensive care unit patients were at three times the risk of experiencing an estimated GFR drop of 30% or more.
Al-Aly explained, “The kidney damage was over-reduced function caused by normal aging. A 60-year-old’s kidney function is less robust than the kidneys of a 20-year-old. The kidney function decline we’ve observed in these patients is not graceful aging. It is not normal anything. It is a disease state.”
“Kidney disease is one important facet of the multifaceted long COVID-19. It is a critical component of the long COVID-19 story, and it must be taken into account when caring for people with long COVID-19.”
Journal Reference:
- Bowe B, Xie Y, Xu E, Al-Aly Z. Kidney Outcomes in Long COVID. Journal of the American Society of Nephrology. Published online Sept. 1, 2021. DOI: 10.1681/ASN.2021060734