CD8+ T cells are vital for immune defense against intracellular pathogens. They play a crucial role in cancer treatments. The cells detect and eliminate intracellular infections and in killing cancer cells.
However, most of the patients do not respond well to the treatments. This lead scientists to investigate CD4 T lymphocytes.
Despite playing a significant role with CD8 T cells, CD4 T lymphocytes’s ability to eliminate tumor cells directly has been a matter of controversy.
In collaboration with Swiss Cancer Centre Léman (SCCL, Switzerland), scientists from universities of Geneva (UNIGE) and Lausanne (UNIL), the Ludwig Institute for Cancer Research (LICR), EPFL and CHUV, investigated when the CD4 T lymphocytes were directly put in close contact to the cancer cells.
Camilla Jandus, last author of the study and a professor in the Department of Pathology and Immunology in UNIGE’s Faculty of Medicine and adjunct scientist at LICR, said, “When cancer cells increase in our bodies, our immune system kicks in. The first line of fighters capable of destroying tumor cells are CD8 T lymphocytes, known as cytotoxic T cells, backed up by CD4 T lymphocytes. The latter secrete factors that help the former in many ways. That’s why lots of cancer treatments are based on CD8 T lymphocytes.”
“Unfortunately, some patients don’t respond to these treatments, and so we have to find new ones.”
Pedro Romero, a professor in the Department of Fundamental Oncology in UNIL’s Faculty of Medicine and Biology, explains said, “We focused on CD4 T lymphocytes, which offer invaluable support to our immune system. These have a much wider spectrum of functional specializations than CD8 T lymphocytes. For a long time, we didn’t know for sure whether they could differentiate into killer lymphocytes.”
Scientists studied CD4 T lymphocytes from around twenty patients with melanoma who were being treated at CHUV.
For the study, scientists examined CD4 T lymphocytes from around twenty patients with melanoma treated at CHUV. Melanoma is the deadliest cancer that is particularly sensitive to immunotherapies. Scientists isolated the CD4 T lymphocytes from both the blood and fragments of the tumors with the idea of comparing them directly. Dissociated tumor cells and CD4 T cells were co-incubated to observe their behavior individually. Observation tools were then required to provide highly-advanced resolution down to the single-cell level.
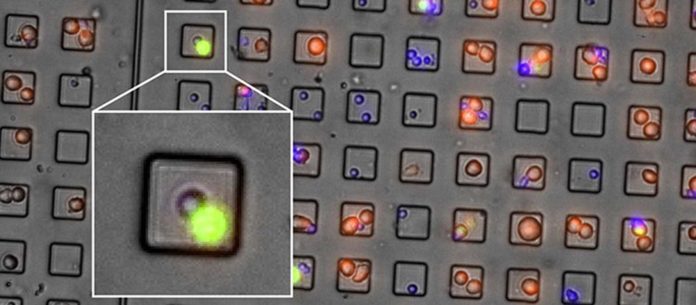
Hatice Altug, a professor in EPFL’s Bionanophotonic Systems Laboratory, said, “We created chips of over 20,000 mini-wells of 65 picolitres (1 picolitre = 10-12 liter) that can accommodate a CD4 T cell and a tumor cell in each of them, and function like boxing rings.”
By photographing all the cells simultaneously every five minutes for 24 hours, scientists observed the interactions between the two cells from a large set of pairs.
Professor Altug said, “We know that it takes about two and a half hours for a CD8 to kill a tumor cell, and we decided to observe these boxing rings for 24 hours without knowing how, and if, the CD4s would react.”
Professor Romero stresses, “the high-throughput integration of dynamic imaging data showed that up to a third of the CD4 T lymphocytes succeeded in killing the tumor cell to which they were closely linked within five hours. These direct observations at the level of individual lymphocytes, which were revealed for the first time at such a level of sensitivity, definitively confirm the existence of CD4 T lymphocytes capable of killing tumor cells. And this happens while the tumor cells sometimes manage to divert them from their function of providing protective support to make allies of them.”
While observing killer variety of CD4 T lymphocytes in detail, scientists demonstrated that they expressed the SLAMF7 molecule, which promoted their tumor killer activity.
Dr. Jandus said, “That’s why we’re now going to isolate and cultivate in vitro the best killer variety of CD4 T lymphocytes so we can turn them into a veritable army of trillions of cells, which we can then inject into patients on whom CD8-based treatments don’t work. The human body naturally has only a small number of CD4 T lymphocytes directed against tumors and not enough to defeat them. The ability to visualize this close combat with our picowell chip paves the way for expanding the arsenal in the fight against cancer, which we now need to develop.”
Journal Reference:
- Amélie Cachot et al. Tumor-specific cytolytic CD4 T cells mediate immunity against human cancer. DOI: 10.1126/sciadv.abe3348