Craniosynostosis, a condition where a baby’s skull fuses too early, is caused by too many of a new kind of bone-forming cell, say researchers from Weill Cornell Medicine. This condition happens because of specific gene changes and affects about one in 2,500 babies. When the skull closes too soon, a baby’s brain can grow abnormally, and they may need surgery to fix it. In tough cases, they might need more than one surgery.
In a study published in Nature on September 20, researchers investigated how a common mutation seen in human craniosynostosis affects the skulls of mice. They discovered that this mutation causes the early fusion of heads by making a previously unknown type of bone-forming stem cell, called DDR2+ stem cells, multiply abnormally.
Study co-senior author Dr. Matt Greenblatt, an associate professor of pathology and laboratory medicine at Weill Cornell Medicine and a pathologist at NewYork-Presbyterian/Weill Cornell Medical Center, said, “We can now start to think about treating craniosynostosis not just with surgery but also by blocking this abnormal stem cell activity.”
In a 2018 study published in Nature, Drs. Debnath and Greenblatt and their team discovered a bone-forming stem cell called CTSK+ stem cells. These cells are found in the top part of a mouse’s skull, called the ‘calvarium,’ and the researchers suspected they might be related to causing craniosynostosis.
Their latest research looked into this possibility by modifying mice to have CTSK+ stem cells without one of the genes that usually prevents craniosynostosis. They thought deleting this gene might make these skull stem cells produce too much bone, causing it to fuse the soft, flexible parts of the head called sutures, which are meant to expand in babies.
Dr. Debnath said, “We were surprised to find that, instead of the mutation in CTSK+ stem cells leading to these stem cells being activated to fuse the bony plates in the skull as we expected, mutations in the CTSK+ stem cells instead led to the depletion of these stem cells at the sutures—and the greater the depletion, the more complete the fusion of the sutures.”
The unexpected discovery made the researchers think that another bone-making stem cell might be causing the strange fusion of sutures. After more experiments and a close look at the cells where the fusion was happening, they found the answer: the DDR2+ stem cell. These stem cells, and their offspring build bone differently from the CTSK+ cells.
Usually, the CTSK+ cells keep the DDR2+ cells in check. But when the gene causing craniosynostosis mutates, the CTSK+ cells die off, letting the DDR2+ cells grow uncontrollably.
To understand these stem cells in humans, the researchers teamed up with doctors who specialize in craniosynostosis, including Dr. Caitlin Hoffman, Dr. Elizabeth Ross, and Dr. David Pisapia from Weill Cornell Medicine and Dr. Thomas Imahiyerobo from Columbia University Vagelos College of Physicians and Surgeons.
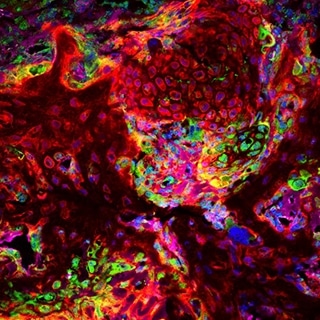
The researchers also found similar DDR2+ and CTSK+ stem cells in human skull samples from craniosynostosis surgeries, showing that their discoveries in mice could be important for treating humans.
Their findings suggest that stopping the DDR2+ stem cells from growing too much might be a treatment in babies with craniosynostosis-related gene mutations. This could be done by copying how CTSK+ stem cells naturally prevent DDR2+ stem cells from expanding. The CTSK+ cells do this by releasing a protein called IGF-1, which helps control the growth of the DDR2+ cells.
Dr. Seoyeon Bok, one of the researchers, said, “We saw that we could partially stop skull fusion by adding IGF-1 over the skull.”
Dr. Greenblatt, another researcher, added, “I can imagine using drugs to control DDR2+ stem cells, along with surgery, to reduce the number of surgeries or improve the results.”
Besides focusing on treatments, the researchers are also looking for more types of bone-making stem cells in the skull. Dr. Greenblatt said, “This study has shown that the skull is more complex than we thought, and we believe there might be even more types of stem cells involved.”
In conclusion, the discovery of the DDR2+ stem cell and its role in craniosynostosis significantly advances our understanding of this condition. It offers hope for more effective treatments and underscores the need for continued research to unlock the full complexity of the cranial bone development process.
Journal Reference:
- Bok, S., Yallowitz, A.R., Sun, J. et al. A multi-stem cell basis for craniosynostosis and calvarial mineralization. Nature. DOI: 10.1038/s41586-023-06526-2.
