The mammalian fetus is dependent upon the placenta for nutrients and oxygen.
The placenta is a specialized organ that contains cells from both baby and mother.
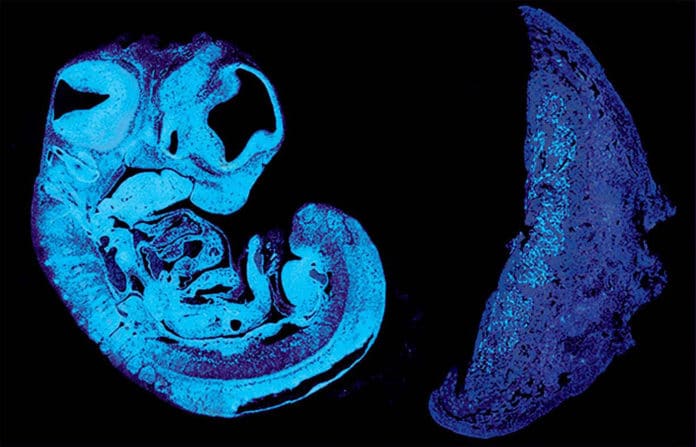
Between 10% and 15% of babies grow poorly in the womb, often showing reduced growth of blood vessels in the placenta. In humans, these blood vessels expand dramatically between mid and late gestation, reaching a total length of approximately 320 kilometers at term.
Cambridge scientists have identified a key signal that the fetus uses to control its supply of nutrients from the placenta.
It reveals a tug-of-war between genes inherited from the father and the mother. The study, carried out in mice, could help explain why some babies grow poorly in the womb.
In a study published today in Developmental Cell, a team led by scientists at the University of Cambridge used genetically engineered mice to show how the fetus produces a signal to encourage the growth of blood vessels within the placenta. This signal also causes modifications to other placenta cells to allow more nutrients from the mother to go through to the fetus.
The researchers used mice, as it is possible to manipulate their genes to mimic different developmental conditions. This enables them to study in detail the different mechanisms taking place. The physiology and biology of mice have many similarities with those of humans, allowing researchers to model human pregnancy to understand it better.
“Although a vast number of genetic pathways have been discovered that are important for the development of different cell types in the placenta and the fetus, there are no functional genetic investigations to date on how the fetus signals its nutrient requirements to the placenta and how the placenta matches these demands.” Study quotes
Dr. Ionel Sandovici, the paper’s first author, said: “As it grows in the womb, the fetus needs food from its mum, and healthy blood vessels in the placenta are essential to help it get the correct amount of nutrients it needs.”
“We’ve identified one way that the fetus uses to communicate with the placenta to prompt the correct expansion of these blood vessels. When this communication breaks down, the blood vessels don’t develop properly, and the baby will struggle to get all the food it needs.”
The team found that the fetus sends a signal known as IGF2 that reaches the placenta through the umbilical cord. In humans, levels of IGF2 in the umbilical cord progressively increase between 29 weeks of gestation and term: too much IGF2 is associated with too much growth, while not enough IGF2 is associated with too little growth. Babies that are too large or too small are more likely to suffer or even die at birth and have a higher risk of developing diabetes and heart problems as adults.
Dr Sandovici added: “We’ve known for some time that IGF2 promotes the growth of the organs where it is produced. In this study, we’ve shown that IGF2 also acts like a classical hormone – it’s produced by the fetus, goes into the fetal blood, through the umbilical cord and to the placenta, where it acts.”
Their findings are fascinating about the tussle taking place in the womb.
In mice, the response to IGF2 in the placenta’s blood vessels is mediated by another protein called IGF2R. The two genes that produce IGF2 and IGF2R are ‘imprinted’ – a process by which molecular switches on the genes identify their parental origin and can turn the genes on or off. Only the copy of the igf2 gene inherited from the father is active, while only the one of igf2r inherited from the mother is active.
Lead author Dr Miguel Constância, said: “One theory about imprinted genes is that paternally-expressed genes are greedy and selfish. They want to extract the most resources as possible from the mother. But maternally-expressed genes act as countermeasures to balance these demands.”
“In our study, the father’s gene drives the fetus’s demands for larger blood vessels and more nutrients, while the mother’s gene in the placenta tries to control how much nourishment she provides. There’s a tug-of-war taking place, a battle of the sexes at the level of the genome.”
The team says their findings will allow a better understanding of how the fetus, placenta, and mother communicate during pregnancy. This, in turn, could lead to ways of measuring levels of IGF2 in the fetus and finding ways to use medication to normalise these levels or promote normal development of placental vasculature.
“Our findings suggest that poor placentation in humans could be caused by deficient microvasculature expansion due to reduced fetus-derived IGF2 signaling, with important clinical implications.” Study quotes
The lead researchers are the Department of Obstetrics and Gynaecology, the Medical Research Council Metabolic Diseases Unit, part of the Wellcome-MRC Institute of Metabolic Science, and the Centre for Trophoblast Research, all at the University of Cambridge.
Journal Reference
- Sandovici, I et al. The Imprinted Igf2-Igf2r Axis is Critical for Matching Placental Microvasculature Expansion to Fetal Growth. Developmental Cell; 10 Jan 2022: DOI: 10.1016/j.devcel.2021.12.005