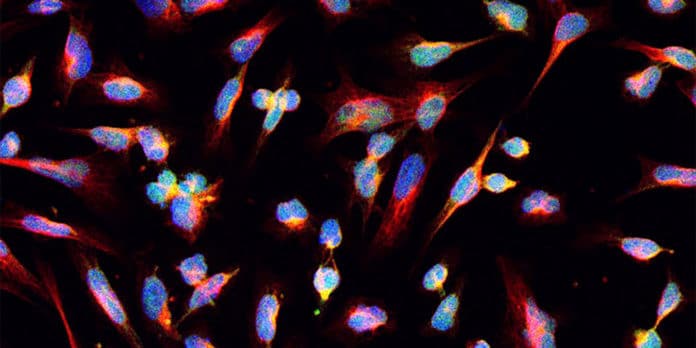
Gliomas are primary brain tumors that display histologic features of glial cells. Diffuse gliomas are the most common types and generally affect the cerebral hemispheres of adults.
In a new study, scientists at the University of Leeds have determined why it is so challenging to treat diffuse glioma. The findings suggest that when tumors are treated with radiation or chemotherapy, their cells evolve in a way that appears to be random.
A total of 222 adult patients with glioma were involved in the study. Scientists collected tumor samples at multiple time points during treatment to understand how the tumors evolved in response to therapy. By analyzing mutations and copy numbers across the three major subtypes of diffuse glioma, they found that driver genes detected at the initial stage of the disease were retained at recurrence. In contrast, there was little evidence of recurrence-specific gene alterations.
Co-author Dr. Lucy Stead, from the University of Leeds’ School of Medicine, said: “These findings show why gliomas are so hard to treat. In other cancers, cells with certain mutations were found to resist treatment, and discovering those mutations allowed new drugs to be developed. Unfortunately, in glioma, where tumor regrowth after treatment is almost universal, we have not found any such mutations.”
“However, this database can now act as a reference for researchers and clinicians to study glioma evolution in response to treatment.”
“The database could help predict how effective new cancer treatments might be at tackling brain tumors, enabling us to prioritize the development of those that are most likely to succeed.”
The recurrence of Glioma is inevitable; its management is often unclear and case-dependent. Be that as it may, while the initial molecular characteristics have been very much depicted in gliomas, their ensuing advancement under treatment remained obscure.
To address this problem, an international community of clinicians and researchers established the Glioma Longitudinal Analysis (GLASS) Consortium, which is investigating the dynamics of molecular changes in gliomas over time.
Lead researcher Dr. Roel Verhaak, from The Jackson Laboratory in the USA, said: “More data are needed to understand glioma evolution fully, but the GLASS resource provides an excellent foundation to more effectively study both evolution and treatment response.”
“Collectively, these findings will help us determine what treatment approaches will result in the greatest removal or killing of glioma cells possible.”
The approach of rigorous molecular examination has demonstrated that the situation is unquestionably progressively complex and that there can be many sub-clonal cell populaces even inside a single tumor.
That makes a significant issue for effective treatment: destroying one sort of cancer cell may leave another unaffected, and it might confer a competitive advantage to it.
During the study, scientists demonstrated that when glioma cells were stressed by cancer therapies such as radiation and chemotherapy, they did not evolve consistently.
They found some common highlights between patient samples, for example, hypermutation- an exceptionally high pace of mutation in the genome- and aneuploidy – in which whole chromosomes were lost or procured through cell division errors.
Following early events that drove cancer initiation and progression, the analysts found that the evolution of tumors frequently had all the earmarks of being random instead of proceeding down predictable paths.
Scientists also assessed how immune activity could shape glioma evolution. They showed that immune activity doesn’t vary in glioma over time, though there were patient-to-patient differences, and more work is needed to fully understand the variability and what immunotherapy strategies might be most effective for gliomas.
Scientists identified a particular mutation in the gene IDH1 that produces a neoantigen – a potential immune system target – and persisted through recurrence. The finding provides a possible opening for vaccine treatment at both the initial and recurrent stages of glioma.
Dr. Stead added: “Other researchers are currently trying to develop IDH1 vaccines and clinical trials are underway.”
“Our results suggest we can have more confidence that these trials may succeed, which is particularly important given that survival for brain tumors has not increased for decades.”
The research was carried out at the University of Leeds and Leeds Cares and the PPR Foundation-funded Leeds Teaching Hospitals NHS Trust.
Kevin Gerrie, Director of Fundraising at Leeds Cares, said it was vital that the charity was able to invest in research like this. He said: “Pilot grants like that given to support Dr. Stead are significant to support the world-class research that takes place here in Leeds.”
“Our donors and supporters will be delighted to know that this work will provide crucial insights into the treatment of those with malignant brain tumors.”