Autoimmune diseases are a common cause of delayed wound healing. These wounds significantly impact mortality psychosocial wellbeing and quality of life.
In normal healing, wounds progress through four overlapping phases: hemostasis, inflammation, proliferation, and remodeling to restore epithelial integrity. Chronic wounds, however, are often arrested in the inflammatory phase and are unable to transition to the proliferation phase with concurrent upregulation of angiogenesis and matrix deposition.
Now, UNIST scientists have discovered a new way that will make faster healing of wounds by regulating cells that orchestrate the inflammatory response. They demonstrated that SREBP-2 protein plays a vital role in cholesterol-related genes, regulates the function of macrophages in the inflammatory response.
In patients with chronic inflammation, for example, rheumatism, recovery by the macrophages (late irritation) isn’t performed appropriately. Inflammation in the existing patient’s body disrupts the treatment course.
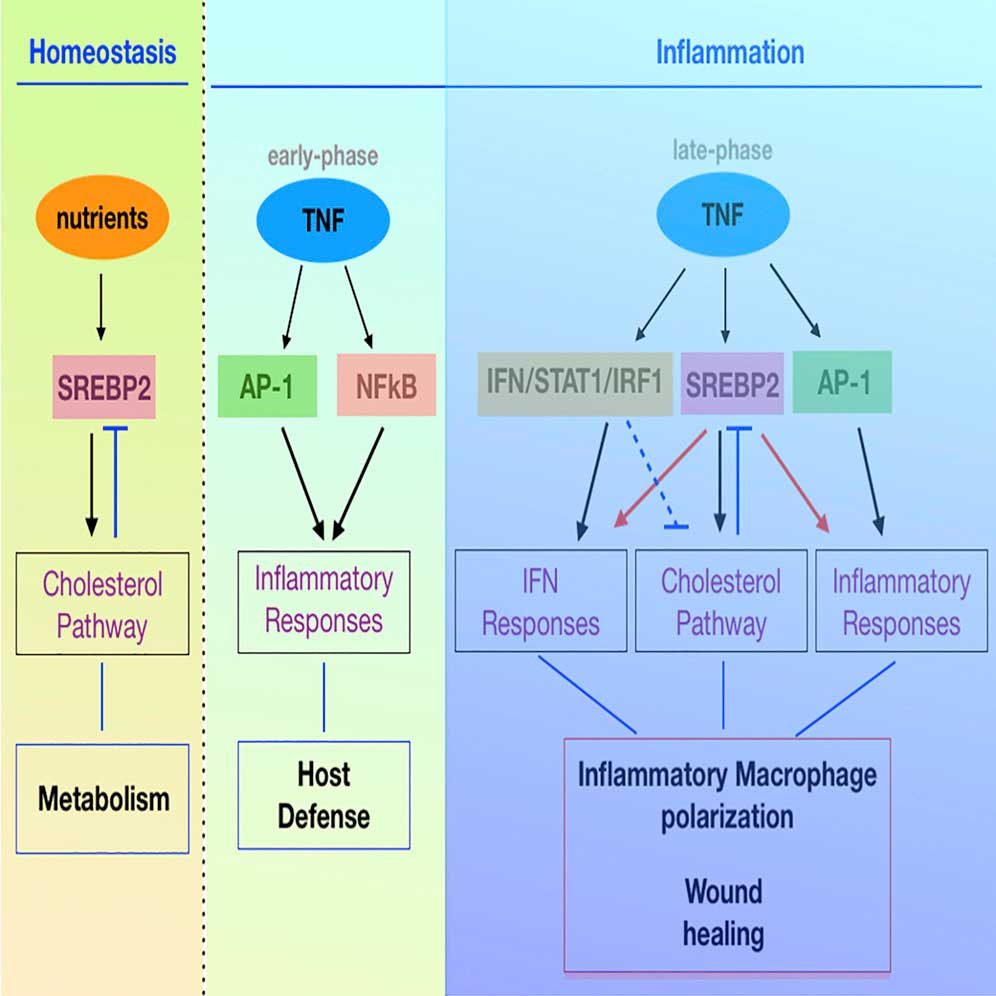
In wound healing, inflammatory mediators are used to bringing inflammatory cells into the wound. TNF (Tumor Necrosis Factor) is a representative of a variety of inflammatory cells, including macrophages. However, the macrophage activation response by TNF is mainly studied in the early stages of inflammation (harmful treatment), so the mechanism of late inflammation (regeneration), which is essential for wound healing, is not well known.
Scientists discovered that the TNF increases SREBP2 protein as the inflammatory response develops. The protein ties to inflammatory target genes and supports the inflammatory response incited by macrophages, easing wound healing.
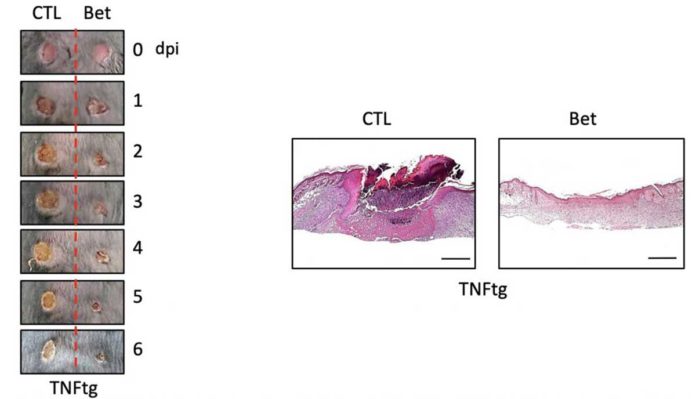
Inhibiting the activity of SREBP2 protein can promote macrophage regeneration. During experiments, the wound recovery and the rate of improvement in the skin of mice that locally inhibited the production of SREBP2 and the control rats were faster, and the wounds of mice that inhibited the production of SREBP2 were faster.
Professor Sung Ho Park in the School of Life Sciences at UNIST said, “Our study uncovers new features of the SREBP2 protein, known to regulate cholesterol metabolism, and reveals wound healing mechanisms. It is significant that the company has discovered a new target material for the development of wound treatments for autoimmune diseases in the future.”
The study is published in the international journal in the field of immunology.