Researchers at Stanford Medicine of Stanford University discovered that a small molecule can make older or injured mice stronger. This molecule fixes the connections between nerves and muscles lost over time. They found that this molecule blocks an enzyme called 15-PGDH, which increases in aging muscles. The study also revealed that this enzyme increases after nerve damage and is common in people with muscle diseases.
This research is the first to show that damaged nerve connections between the spinal cord and muscles can be encouraged to heal with a drug. This means that lost muscle strength and mass can be partly restored. If similar results are found in humans, this drug could one day help prevent muscle loss due to aging or disease and speed up recovery from injuries.
Helen Blau, Ph.D., professor of microbiology and immunology, said, “There is an urgent, unmet need for drug treatments that can increase muscle strength due to aging, injury or disease. This is the first time a drug treatment has been shown to affect both muscle fibers and the motor neurons that stimulate them to contract to speed healing and restore strength and muscle mass. It’s unique.”
Professor Blau, the Baxter Laboratory Director, led the study published in Science Translational Medicine on Oct. 11. The lead authors are Dr. Mohsen Bakooshli, a postdoctoral scholar, and Dr. Yu Xin Wang, a former postdoctoral scholar. Dr. Wang is currently an assistant professor at the Sanford Burnham Prebys Medical Discovery Institute in San Diego.
The Blau laboratory researches how muscles weaken due to aging and diseases and whether they can be prevented. In a previous study from 2021, they found that blocking an enzyme called 15-PGDH in older mice made them stronger. They’ve discovered that this effect happens because it repairs the connections between nerves and muscles needed for muscle contractions. These connections, called neuromuscular junctions, deteriorate as we age, weakening muscles. People usually lose muscle mass and strength, about 10% per decade, after turning 50.
Other factors, like inactivity due to illness or muscle-wasting diseases, can also harm these connections. In earlier research, they found that PGE2 is crucial for muscle repair. They realized that 15-PGDH, which breaks down PGE2, increases in muscles as we age. Blocking this enzyme can counteract the strength loss associated with aging.
Blau said, “PGE2 is part of the body’s natural healing mechanism, and its levels increase in muscle after injury. We wanted to learn how age triggers an increase in 15-PGDH, and therefore the degradation and loss of PGE2.”
The researchers noticed that their muscles lose nerve connections as people and animals age. They wondered if this loss might be linked to the increased levels of 15-PGDH.
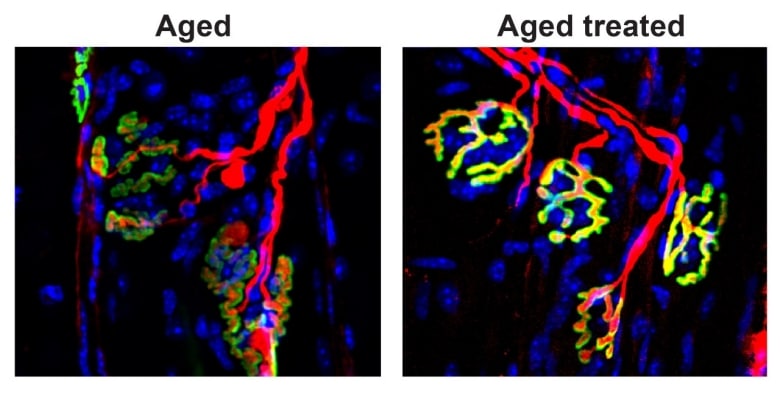
Their experiments found that when they cut the nerves that connect to leg muscles in mice, the levels of 15-PGDH in the muscles shot up quickly. What excited them even more, was that when they treated these mice with a drug that stops 15-PGDH, the nerves regrew faster and made contact with the muscles more quickly than in untreated mice. This led to a quicker recovery of strength and function.
Further tests showed that the drug restored lost connections between nerves and muscles, increased muscle strength, and improved function in old mice. They also found clumps of 15-PGDH in the muscle fibers of people with neuromuscular disorders, suggesting a possible link to these conditions.
The researchers plan to delve deeper into how blocking 15-PGDH stimulates nerve growth at a molecular level. They’ve even co-founded a company, Epirium Bio, to develop similar drugs for human use. While they’re still doing animal studies, the company hopes to start a clinical trial in the next year or so.
Blau said, “Our next steps will be to examine whether blocking 15-PGDH function in people with spinal muscular atrophy can increase lost muscle strength in combination with gene therapy or other treatments. We are also looking at ALS to see if something like this might help these patients. It’s fascinating that we can affect muscle function and motor neuron growth.”
The research received support from various sources, including the National Institutes of Health, the Canadian Institutes of Health, and several foundations and institutes.
Helen Blau holds patents related to this research. She is involved with Epirium Bio, a company working on 15-PGDH inhibition for enhancing muscle strength.
The Stanford Medicine study’s groundbreaking findings offer hope in the fight against muscle frailty and provide valuable insights into restoring nerve-muscle connections in aging individuals. These results hold promise for developing therapeutic interventions to address age-related muscle weakness and various neuromuscular disorders in the future.
Journal reference:
- Mohsen A. Bakooshil, , Yu Xin Wang etal., After acute and chronic denervation by inhibiting the gerozyme 15-prostaglandin dehydrogenase, regenerating neuromuscular synapses. Science Translational Medicine. DOI: 10.1126/scitranslmed.adg1485.
