A team of scientists at the Northwestern University has devised a pair of soft, flexible, wireless body sensors that holds the potential to replace the tangle of wire-based sensors that currently monitor babies in hospitals’ neonatal intensive care units (NICU) and pose a barrier to parent-baby cuddling and physical bonding.
The sensors offer precise data and also are gentler on a newborn’s fragile skin and allow for more skin-to-skin contact with the parent.
Four essential advances serve as the foundations for this technology:
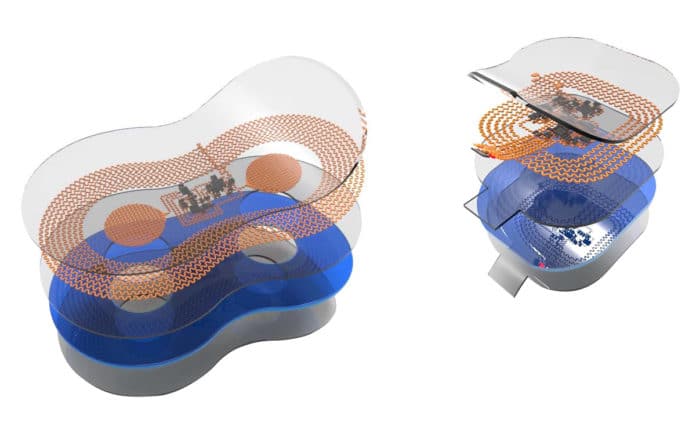
1. Schemes for wireless power transfer, low-noise sensing, and high-speed data communications via a single radio-frequency link with negligible absorption in biological tissues
2. Efficient algorithms for real-time data analytics, signal processing, and dynamic baseline modulation implemented on the sensor platforms themselves
3. Strategies for time-synchronized streaming of wireless data from two separate devices
4. Designs that enable visual inspection of the skin interface while also allowing magnetic resonance imaging and x-ray imaging of the neonate
The study includes initial data from more than 20 babies who wore the wireless sensors alongside traditional monitoring systems, so Northwestern researchers could do a side-by-side, quantitative comparison. Since then, the team has conducted successful tests with more than 70 babies in the NICU.
John A. Rogers, a bioelectronics pioneer, who led the technology development said, “We wanted to eliminate the rat’s nest of wires and aggressive adhesives associated with existing hardware systems and replace them with something safer, more patient-centric and more compatible with parent-child interaction.”
“Our wireless, battery-free, skin-like devices give up nothing in terms of the range of measurement, accuracy, and precision — and they even provide advanced measurements that are clinically important but not commonly collected.”
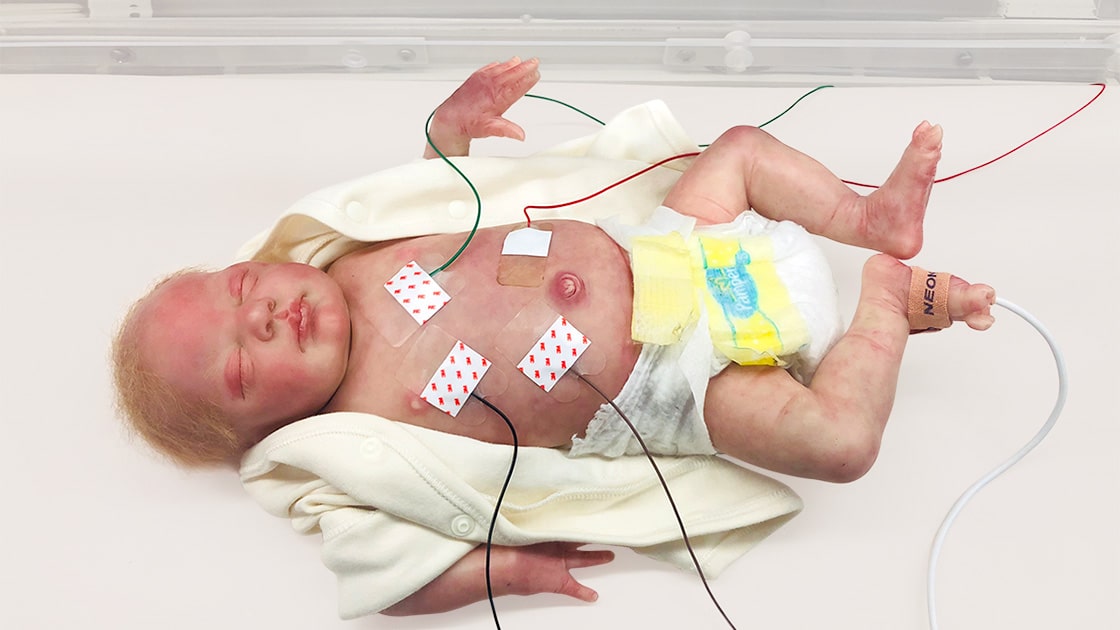
Northwestern University, Wireless infant sensors, The mass of wires that surround newborns in the NICU are often bigger than the babies themselves. Typically five or six wires connect electrodes on each baby to monitors for breathing, blood pressure, blood oxygen, heartbeat and more. Although these wires ensure health and safety, they constrain the baby’s movements and pose a major barrier to physical bonding during a critical period of development.
Dr. Amy Paller, a pediatric dermatologist said, “We know that skin-to-skin contact is so important for newborns — especially those who are sick or premature. It’s been shown to decrease the risk of pulmonary complications, liver issues, and infections. Yet, when you have wires everywhere and the baby is tethered to a bed, it’s really hard to make skin-to-skin contact.”
Pediatrician Dr. Debra Weese-Mayer said, “Anybody who has had the experience of entering a NICU immediately notices how tiny the babies are, and how many wires and electrodes are attached to them. The opportunity to go wireless has enormous potential for decreasing the burden for the nurses, for the babies and for the parents.”
The sensors work by monitoring babies’ vital signs — heart rate, respiration rate,
and body temperature — from opposite ends of the body. One sensor lies across the baby’s chest or back, while the other sensor wraps around a foot. This strategy allows physicians to gather an infant’s core temperature as well as body temperature from a peripheral region.
The wireless sensor communicates through a transmitter placed underneath the crib’s mattress. Using radio frequencies the same strength as those in RFID tags, the antenna transmits data to displays at the nurses’ station.
Both sensors are placed at different locations on the body because differences in temperature between the foot and the chest have great clinical importance in determining blood flow and cardiac function.
Scientists noted, “The device also could help fill in information gaps that exist during skin-to-skin contact. If physicians can continue to measure infants’ vital signs while being held by their parents, they might learn more about just how critical this contact might be. Transparent and compatible with imaging, the sensors also can be worn during X-rays, MRIs and CT scans.”
In the case of premature babies, existing technology could damage the skin that may also lead to lifelong scarring. Scientists studied 70 babies in the NICU thus far and found no sign of skin damage from the wireless sensors. The sensor’s skin-saving secret lies in its lightweight nature, thin geometry, and soft mechanics. The paper-thin device is made from biocompatible, soft elastic silicone that embeds a collection of tiny electronic components connected with spring-like wires that move and flex with the body.