A recent outbreak in India of Nipah virus encephalitis, an often-lethal viral disease with no cure, has set off international alarms over the virus’s potential to become the next threat to global health.
Nipah outbreaks start with a spillover of the virus from its natural reservoir—in this case, giant fruit bats, which don’t get sick from it—to either humans or livestock that come into contact with people. Once the virus gets into people, it can spread from person to person through close contact with bodily fluids, typically from people who are very sick with Nipah to the family members or health-care workers caring for them.
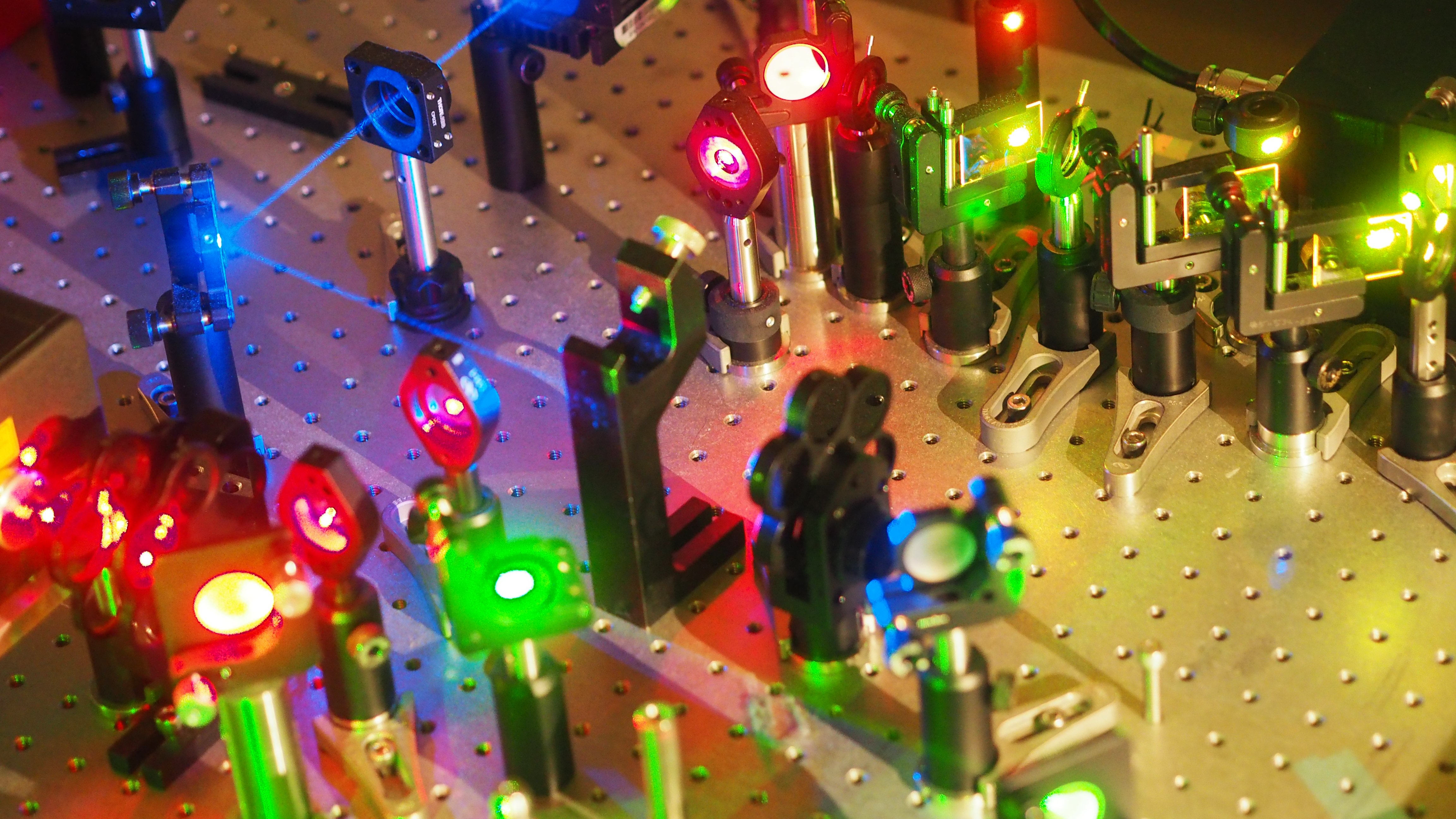
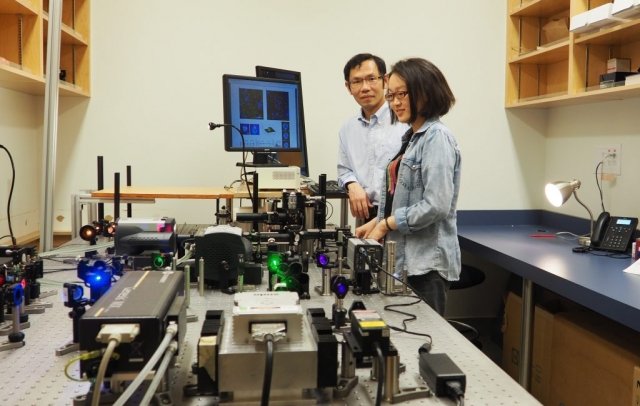
Now, scientists at the University of British Columbia have discovered that the Nipah virus and other similar viruses assemble themselves in a much more haphazard manner than previously thought. They made this discovery using their newly developed optical super-resolution microscope.
Currently, there is no Nipah vaccine approved for human use. One of the potential strategies under development is to use virus-like-particles, which are protein-based structures that mimic viruses, to stimulate an immune response. According to scientists, this discovery could enable scientists to build more effective vaccines and rule out many approaches to fighting these viruses.
Chemistry professor Keng Chou reported, “We looked at hundreds of images, and we couldn’t find anything that supported the current model. For some of these deadly viruses, the replication process is actually not as complicated as some thought.”
He further explained, “Nipah is a case of an “enveloped” virus, which gets its external wrapping from the contaminated host cell, much like the infections that reason influenza, rabies, measles, and AIDS. Nipah can cause extreme illnesses and fatal brain swelling in both humans and animals. Yearly outbreaks in Southeast Asia kill 40 to 90 % of those infected. In 2018, just two out of 19 individuals contaminated by Nipah in India survived an outbreak.”
Nipah infection has three structural proteins: a grid protein that gives structure, and two envelope proteins that empower the infection to join and fuse with host cells. Researchers have trusted those matrix proteins “recruit” envelope proteins, conveying a type of flag so they would all be able to combine on the cell membrane and turn into a functional virus. Scientists have endeavored to distinguish this signal with expectations of discovering approaches to disrupt the process.
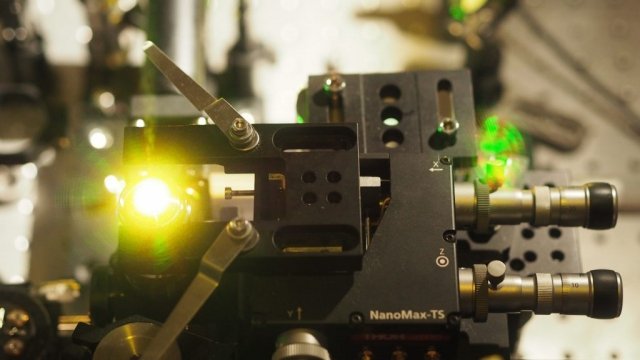
Although, scientists observed that envelope proteins tend to be scattered randomly on the cell membrane. Thus, these proteins are gotten simply by chance when they are fused into a virus. This generates virus particles more rapidly than beforehand imagined, yet numerous matrix proteins don’t get the envelope proteins by any means and don’t become a functional virus.
Qian Liu, a postdoctoral fellow in UBC said, “If a vaccine contains a large percentage of virus-like particles that have only the matrix protein but not the envelope proteins, it won’t trigger a strong immune response to the proteins that are most essential for helping a virus enter cells. Vaccines could be made more effective if we find a way to exclude those non-functional particles from the mix.”
The study, supported by the Natural Sciences and Engineering Research Council of Canada and the Canada Foundation for Innovation, was published earlier this month in Nature Communications.