The study which conducted on mice suggests skin cells that are re-programmed into brain stem cells, transplanted into the central nervous system, help reduce inflammation. It also holds the potential of repairing damage caused by multiple sclerosis (MS).
Through this study, scientists actually wanted to develop personalized treatments based on a patient’s own skin cells for diseases of the central nervous system (CNS).
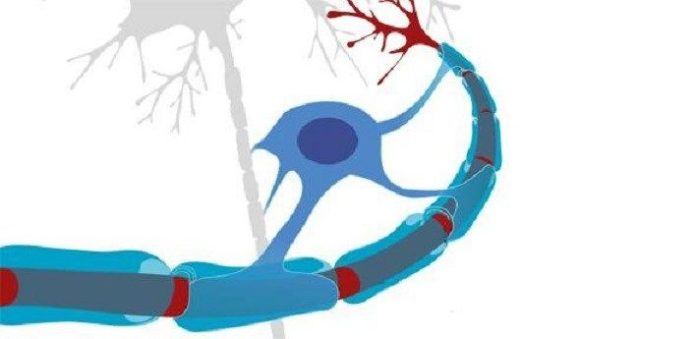
During progressive MS, the immune system harm myelin, the protective sheath around nerve fibers. Thus, it leads to disruption to messages sent around the brain and spinal cord. Symptoms are eccentric and incorporate issues with versatility and adjust torment and serious weariness.
Enter resistant cells engaged with causing this harm are macrophages (actually ‘huge eaters’), which customarily serve to assault and free the group of undesirable interlopers. A specific sort of macrophage known as microglia are found all through the cerebrum and spinal string – in dynamic types of MS, they assault the CNS, making incessant irritation and harm nerve cells.
Late advances have raised desires that ailments of the CNS might be enhanced by the utilization of undifferentiated cell treatments. Undifferentiated organisms are the body’s ‘lord cells’, which can form into a cell inside the body. Past work from the Cambridge group has demonstrated that transplanting neural undeveloped cells (NSCs) – immature microorganisms that are part-approach to forming into nerve cells – decreases irritation and can enable the harmed CNS to mend.
In a new study by the University of Cambridge, scientists suggest, iNSCs may be a viable option to repairing some of the damage caused by MS. Utilizing mice that had been controlled to create MS, the analysts found that endless MS prompts essentially expanded levels of succinate, a little metabolite that sends signs to macrophages and microglia, deceiving them into causing aggravation, however just in cerebrospinal liquid, not in the fringe blood.
Transplanting NSCs and iNSCs straightforwardly into the cerebrospinal liquid diminishes the measure of succinate, reinventing the macrophages and microglia – generally, turning ‘terrible’ safe cells ‘great’. This prompts an abatement of irritation and ensuing optional harm to the mind and spinal line.
Dr. Stefano Pluchino, lead author of the study from the Department of Clinical Neurosciences at the University of Cambridge said, “Our mouse study suggests that using a patient’s reprogrammed cells could provide a route to personalized treatment of chronic inflammatory diseases, including progressive forms of MS.”
“This is particularly promising as these cells should be more readily obtainable than conventional neural stem cells and would not carry the risk of an adverse immune response.”
Dr. Luca Peruzzotti-Jametti, the first author of the study and a Wellcome Trust Research Training Fellow, says: “We made this discovery by bringing together researchers from diverse fields including regenerative medicine, cancer, mitochondrial biology, inflammation and stroke and cellular reprogramming. Without this multidisciplinary collaboration, many of these insights would not have been possible.”
Referrance:
Peruzzotti-Jametti, L et al. Macrophage-derived extracellular succinate licenses neural stem cells to suppress chronic neuroinflammation. Cell Stem Cell; 2018; 22: 1-14; DOI: 10.1016/j.stem.2018.01.20