Microneedle sensors could provide minimally invasive, ongoing molecular monitoring, providing real-time information on the status of diseases and their treatments. Pharmaceutical wearable sensors, for instance, would make it possible to tailor treatments to each patient’s pharmacokinetics.
To construct a wearable sensor patch that can continually monitor the levels of one of these medicines, researchers at Sandia National Laboratories coupled previous work on painless microneedles with nanoscale sensors.
According to project leader and Jill Hruby Fellow Alex Downs, the medication they’re following is vancomycin, used as a last resort to treat severe bacterial infections. Vancomycin has a small range within which it successfully kills bacteria without injuring the patient; therefore, continuous monitoring is essential.
Philip Miller, a Sandia biomedical engineer who advised on the project, said, “This is a great application because it requires tight control. In a clinical setting, how that would happen is a doctor would check on the patient on an hourly basis and request a single time-point blood measurement of vancomycin. Someone would come to draw blood, send it to the clinic, and get an answer back at some later time. Our system is one way to address that delay.”
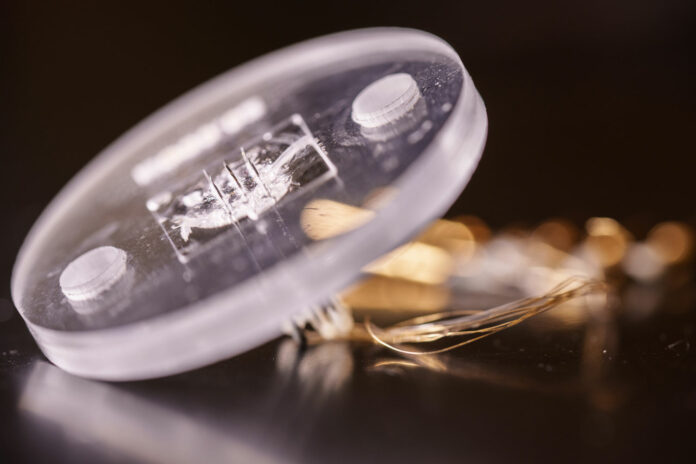
The sensor system begins with an insulin pen-style microneedle that is readily accessible on the market. An angle is cut into one end of a polymer-coated gold wire that is about one-fourth the thickness of a human hair by Sandia materials scientist Adam Bolotsky. The gold wire is then cautiously inserted inside the needle, soldered to a connection, and electrical insulation is made sure of. The researchers use coated silver and platinum wires inside commercial microneedles to make similar reference and counter electrodes.

Sandia technologists Bryan Weaver and Haley Bennett designed a plastic patch the size of a silver dollar. These needles are then inserted into a plastic patch that includes room for nine microneedles but can be adjusted for any number desired.
Downs said, “On each gold wire’s exposed, diagonal surface, the researchers chemically attach the nanoscale sensors.”
The sensors, known as aptamers, are DNA strands with an electrically reactive chemical on one end and a surface linker on the other. According to Downs, the DNA changes its form when it binds to the antibiotic vancomycin, moving the electrically sensitive molecule closer to the gold surface. This movement increases the current that the sensor system is detecting. Electrical detection also shows that some DNA reverts to its native structure as the vancomycin concentration falls.
Downs said, “This reversibility is useful for real-time measurements. If you want to see the concentration of a certain chemical present in the skin or in the blood at any given time, then being able to measure increases and decreases is important.”
“I merged my knowledge of aptamer-based sensing and real-time monitoring with the technology that Ronen Polsky and Phil Miller had developed at Sandia. By integrating these two tools, we substantially miniaturized the sensing system and verified that it worked in a microneedle.”
“After constructing the microneedle sensors, the team tested whether a microneedle sensor could detect vancomycin in a saline solution mimicking the conditions inside the body. Once successful, they tested the entire system, complete with reference and counter electrodes, in a much more complex solution: undiluted cow blood. The system was still able to detect vancomycin.”
The researchers subsequently inserted the patch into pig skin multiple times, watched the electronic signal from the patch while it was in the skin, and assessed its capacity to detect vancomycin to see if the microneedles and aptamers would function after being inserted into the skin.
It was highly unclear whether this would continue to transmit a signal after being inserted into the skin. Every microneedle functions as a separate sensing electrode. This definitely would only work if the sensors were making good electrical contact. We had never tested that at Sandia, making it the biggest unknown.
Miller said, “The next big technical hurdle is proving that it works in the body for an extended amount of time.”
In the future, a similar approach using various DNA aptamers might be used to track cytokines, which are tiny proteins that act as messengers inside the body, as well as other proteins or smaller molecules that undergo significant changes during infections. These methods speed up the diagnosis of a patient’s disease or even help with triage in emergency scenarios.
Additionally, Downs has been researching whether substances in the blood and skin can “clog” the sensors over time, lowering their accuracy. She and her summer intern, Amelia Staats, discovered that the leading cause of signal interference is fibrinogen, a molecule involved in blood clotting. The researchers will release these results in a future study.
Downs said, “This system could be used anywhere where you’re having large chemical changes in the body, where you want to measure those changes over time to understand better what’s happening in the body.”
Journal Reference:
- Alex M. Downs, Adam Bolotsky, Bryan M. Weaver et al. Microneedle electrochemical aptamer-based sensing: Real-time small molecule measurements using sensor-embedded, commercially-available stainless steel microneedles. Biosensors and Bioelectronics. DOI: 10.1016/j.bios.2023.115408