In cell therapy, clinicians reprogram some skin or blood cells from patients to create induced pluripotent stem cells. They coax these stem cells to transform into progenitor cells for treating spinal cord injury. These progenitors are then transplanted back into the patient to regenerate part of the injured spinal cord. However, pluripotent stem cells that don’t entirely change into progenitors can form tumors.
Scientists at MIT and the Singapore-MIT Alliance for Research and Technology have developed a tiny device to improve cell therapy treatments with more excellent safety and effectiveness. They developed a microfluidic cell sorter to remove undifferentiated cells without damaging fully-formed progenitor cells.
This newly developed device can sort more than 3 million cells per minute without special chemicals. In the study, scientists found that combining many devices can sort more than 500 million cells per minute.
Pluripotent stem cells were generally larger than the progenitor cells derived from them. It happens because pluripotent stem cells have many genes that haven’t been switched off in their nucleus. As these cells specialize in specific functions, they suppress many genes that are no longer required, hence shrinking the nucleus. The microfluidic device leverages this size difference to sort the cells.
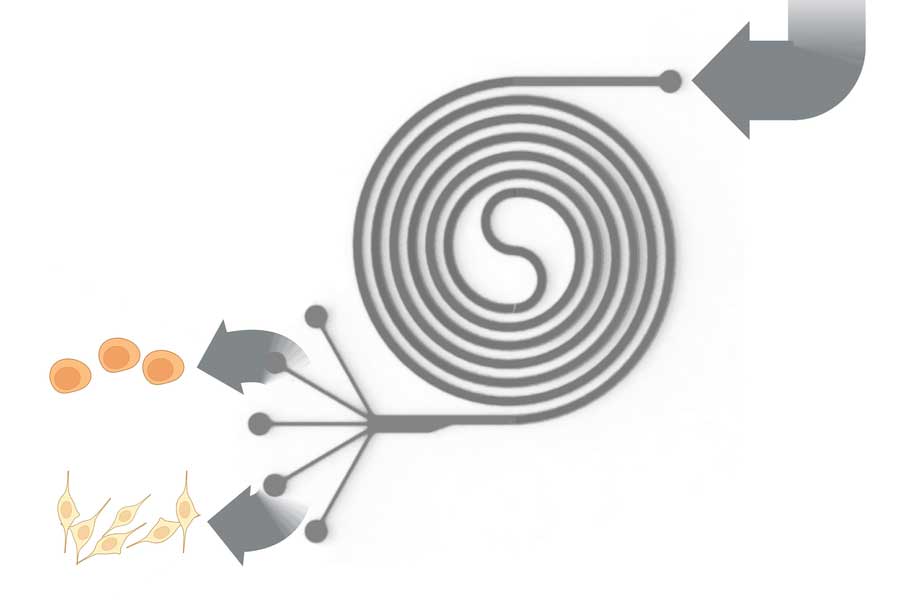
The plastic chip contains tiny channels that create an inlet for cells to enter, a spiral pathway, and four outlets where cells of different sizes are collected. When cells pass through the spiral at high speeds, various forces, including centrifugal forces, push them around. These forces help gather the cells at a specific point in the fluid stream based on their size, effectively separating them into different outlets.
The researchers discovered they could enhance the sorter’s performance by running it twice. First, they operate it at a lower speed, causing more giant cells to stick to the walls while smaller cells are sorted out. Then, they run it faster to separate the larger cells.
The device works similarly to a centrifuge, but it doesn’t need human intervention to collect the sorted cells.
The device could remove almost 50% of larger cells in one pass. What’s more, the device doesn’t use any filtration. The limitations with filters are that they become clogged or break down over time so that a filter-free device can be used for much longer.
Having demonstrated success on a small scale, the researchers are now moving on to larger studies and animal models to determine if the purified cells work better when introduced into living organisms.
Journal Reference:
- Tan Dai Nguyen, Wai Hon Chooi, Hyungkook Jeon, et al. Label-Free and High-Throughput Removal of Residual Undifferentiated Cells From iPSC-Derived Spinal Cord Progenitor Cells. Stem Cells Translational Medicine. DOI: 10.1093/stcltm/szae002
