Vascular dysfunctions are a common feature of multiple age-related diseases. However, modeling healthy and pathological aging of the human vasculature represents an unresolved experimental challenge.
A new study by the Salk Institute offers clues on why blood vessels tend to become leaky and hardened with aging. It also helps scientists identifying new molecular targets to potentially slow aging in vascular cells.
Studies on aging vasculature have been hampered because collecting blood vessel cells from patients is invasive.
Be that as it may, when blood vessel cells are made from stem cells called induced pluripotent stem cells, age-related molecular changes are wiped clean. Thus, most information about how blood vessel cells age originates from observations of how the blood vessels themselves change after some time: veins and arteries become less elastic, thickening, and stiffening. These progressions can add to blood pressure increments and an increased danger of heart disease with age.
In 2k15, scientists have shown that fibroblasts could be directly reconstructed into neurons, avoiding the induced pluripotent stem cells stage that deleted the cells’ aging signatures. The subsequent synapses held their markers of age, letting specialists concentrate on how neurons change with age.
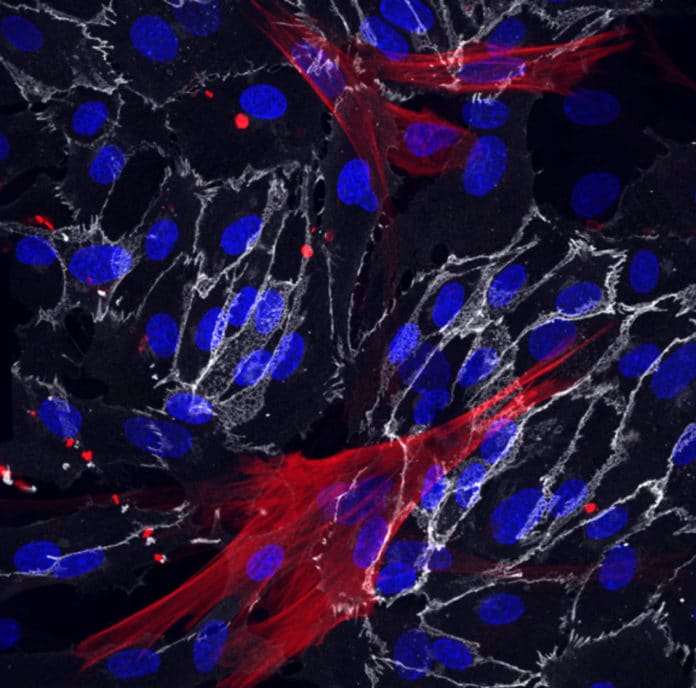
In this study, scientists applied the same direct-conversion approach to creating two types of vasculature cells: vascular endothelial cells, which make up the inner lining of blood vessels, and the smooth muscle cells surrounding these endothelial cells.
Roberta Schulte, the Hetzer lab coordinator and co-first author of the paper, said, “We are among the first to use this technique to study the vascular system’s aging. The idea of developing both of these cell types from fibroblasts was out there, but we tweaked the techniques to suit our needs.”
Scientists used skin cells called fibroblasts from young and old patients to create blood vessel cells that retain their molecular markers successfully. They used skin cells collected from three young donors, aged 19 to 30 years old, three older donors, 62 to 87 years old, and 8 patients with Hutchinson-Gilford progeria syndrome (HGPS), a disorder of accelerated, premature aging often used to study aging.
The resulting induced vascular endothelial cells (iVECs) and induced smooth muscle cells (iSMCs) showed clear age signatures. 21 genes were expressed at different levels in the iSMCs from old and young people, including genes related to the calcification of blood vessels. 9 genes were expressed differently according to age in the iVECs, including genes related to inflammation.
In patients with HGPS, some genes reflected the same expression patterns usually seen in older people, while other patterns were unique. In particular, BMP-4 protein levels, which is known to play a role in the calcification of blood vessels, were slightly higher in aged cells compared to younger cells, but more significantly higher in smooth muscle cells from progeria patients. This suggests that the protein is particularly vital in accelerated aging.
The results not only show how and why blood vessels change with age but also confirmed that the direct-conversion method of creating vascular endothelial and smooth muscle cells from patient fibroblasts allowed the cells to retain any age-related changes.
Simone Bersini, a Salk postdoctoral fellow and co-first author of the paper, said, “We now know we can longitudinally study a single patient during aging or the course of treatment and study how their vasculature is changing and how we might be able to target that.”
Scientists also tested the utility of the new observations by trying whether blocking BMP4 — which had been present at higher levels in smooth muscle cells developed from people with HGPS — could help treat aging blood vessels. In smooth muscle cells from donors with vascular disease, antibodies blocking BMP4 lowered vascular leakiness levels — one of the changes that occur in vessels with aging.
The findings point toward new therapeutic targets for treating both progeria and the regular age-related changes in the human vascular system. They also illustrate that the direct conversion of fibroblasts to other mature cell types — previously successful in neurons and, now, in vascular cells — is likely useful for studying a wide range of aging processes.
Journal Reference:
- Simone Bersini et al. Direct reprogramming of human smooth muscle and vascular endothelial cells reveals defects associated with aging and Hutchinson-Gilford progeria syndrome. DOI: 10.7554/eLife.54383