Chronic hepatic encephalopathy (HE) is a complication of chronic liver disease (CLD) and is characterized by cognitive and motor deficits. While minimal and overt HE may affect 20–70% of patients with CLD, the diagnosis is challenging in its early stages. Tools enabling the detection of new neurometabolic changes in patients may allow for timely intervention, thereby minimizing the number of overt HE episodes and ensuing complications and costs.
Valérie McLin, a professor in the Department of Paediatrics, Gynaecology, and Obstetrics at UNIGE’s Faculty of Medicine and Geneva University Hospitals (HUG), explains: “One of the actors in hepatic encephalopathy is ammonium. Ammonium is a substance produced when proteins break down, some of which is directed to the brain where it is transformed into glutamine – used for the production of neurotransmitters – while the liver filters the other part and excretes in the urine.”
Though if the liver malfunctions, it causes an excess measure of ammonium in the brain, and hence glutamine generation, which can trigger cerebral edema and, sometimes, hepatic encephalopathy. There are as yet two obscure elements: are there other molecular actors in charge of hepatic encephalopathy? To what extent does it take for the brain to be influenced by a liver malfunction?
While trying to answer these questions, scientists at the Universities of Geneva (UNIGE) and Lausanne (UNIL), the Vaud University Hospital Centre (CHUV), the Centre for Biomedical Imaging (CIBM), the Federal Polytechnic School of Lausanne (EPFL) and the University Hospitals of Geneva (HUG), Switzerland, observed rats with chronic liver disease for eight weeks.
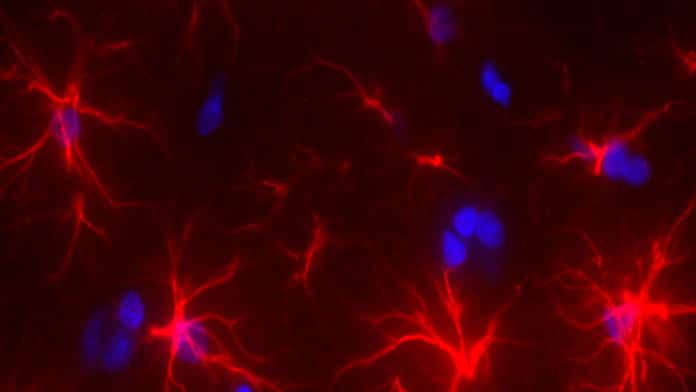
They performed a detailed analysis of hepatic encephalopathy and were able to observe for the first time in a mouse model that a dysfunction of the liver provokes cerebral molecular disturbances in two weeks, even though no physical symptoms are apparent.
Dr. Cristina Cudalbu, a research staff scientist and operational manager of the 9.4T MRI, Center for Biomedical Imaging at EPFL said, “We tracked each animal individually by putting it in a high magnetic field MRI (9.4 Tesla) every two weeks so we could carry out high-resolution spectroscopy (MRS). This meant we could observe the molecular alterations very precisely from the onset of the liver disease. And we discovered hitherto unseen observations!”
“We found that molecular changes affect the brain as early as the second week of liver disease. And yet, the rats have minimal symptoms of the disease. Based on earlier studies, we thought it would take about six weeks to see an impact, i.e., at the beginning of the deterioration of the animal’s health.”
Olivier Braissant, a professor in the Clinical Chemistry Department at CHUV and the Faculty of Biology and Medicine at the University of Lausanne (UNIL) said, “The external signs of the disease appear between the fourth and eighth week: jaundice, malnutrition or water in the belly. From that moment, we observed that in addition to there being an excess of ammonium in the brain, the concentration of the two other molecules drops: vitamin C, an antioxidant, and creatine, which fulfills many functions, including energy-related functions.”
“This is the first time that the role these two new actors play in the disease has been visibly demonstrated. These appear in a second phase after the ammonium in the blood rises.”
The outcomes reveal that an MRS brain scan may identify the neurological manifestations of chronic liver disease well before the presence of the first symptoms. Be that as it may, the scientists likewise expect to know whether it is conceivable to protect the brain from this kind of deterioration – or possibly decrease the harm – by making up for the absence of creatine and vitamin C utilizing supplements or using probiotics.
McLin said, “We are also carrying out similar observations in humans to see whether the brain damage is similar to that in rats.”
The research results are published in the Journal of Hepatology.