Cell membrane engineering is emerging as a premier approach for cell augmentation, as it can be used to rapidly provide additional cell functionality, including immunoevasion, adhesion and homing. However, there are few examples where cell membrane modifications have been used to drive in situ scaffold formation.
In a new study, scientists at the University of Bristol modified the membrane of human mesenchymal stem cells (hMSCs) with an enzyme, known as thrombin, which is involved in the wound healing process.
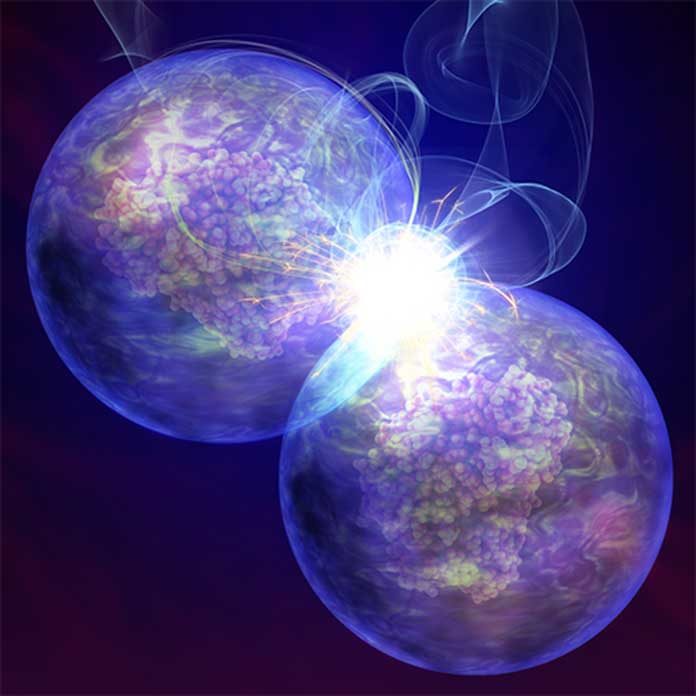
At the point when the modified cells were set in a solution containing the blood protein fibrinogen, they automatically welded together through the development of a natural hydrogel from the surface of the cells. The specialists have additionally demonstrated that the resultant 3D cell structures could be utilized for tissue engineering.
The method involves the synthesis of supercationic thrombin-polymer surfactant complexes that spontaneously bind the plasma membrane of hMSCs and drive in situ fibrin hydrogel nucleation and growth. The resulting self-supporting hydrogel constructs support high levels of metabolic activity and provide a matrix for adipogenic and osteogenic differentiation.
Dr. Adam Perriman, Associate Professor in Biomaterials in the School of Cellular and Molecular Medicine, said: “One of the biggest challenges in cell therapies is the need to protect the cells from aggressive environments after transplantation. We have developed a completely new technology that allows cells to grow their own artificial extracellular matrix, enabling cells to protect themselves and allowing them to thrive after transplantation.”
The team’s findings could increase the possibilities in tissue engineering for chronic wound healing, especially because the process uses fibrinogen, which is abundant in blood.
The researcher’s new method of the conversion of natural enzymes into a membrane binding proteins could pave the way for the development of a wide range of new biotechnologies.
Dr. Perriman said, “We demonstrate that this cell functionalization methodology is facile and can be used to inject thrombin labeled GFP-expressing fibroblasts into an in vivo zebrafish skin wound model.”
The study is published in the journal Nature Communications.