Now, it becomes easy for engineers to study the relationships between different organs and the immune system, thanks to a multitissue model designed by MIT biological engineers on a specialized microfluidic platform seeded with human cells.
This new model is dubbed as “organs-on-a-chip” or “physiome on-a-chip.” Using the model, scientists in this study explored the role of circulating immune cells in ulcerative colitis and other inflammatory diseases. They additionally found that a metabolic byproduct produced by bacteria living in the human gut assumes a significant job under these inflammatory conditions.
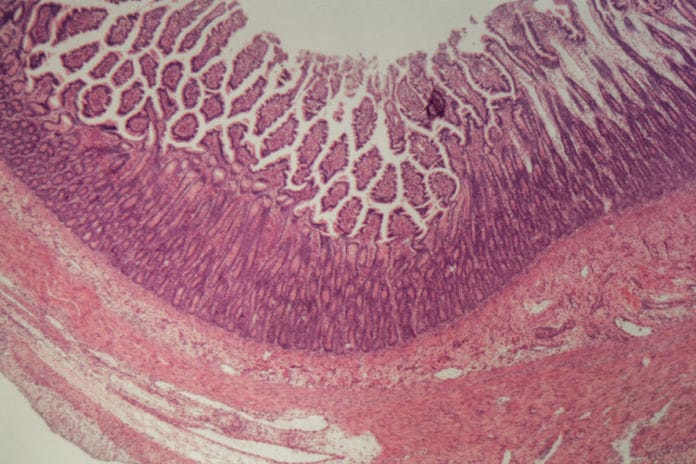
In this study, scientists set out to model interactions between two organs, the colon and the liver. They wanted to examine how the immune system, especially T cells, influences those organs.
It is well known that above 80 percent of patients with a chronic liver autoimmune disease called primary sclerosing cholangitis also suffer from inflammatory bowel disease (IBD). And, patients with IBD have a much greater chance of developing autoimmune disorders of the liver.
The new system contains colon cells taken from patients with ulcerative colitis, along with healthy liver cells. The scientists found that when these tissues were connected, their physiological behavior completely changed as compared to when they are isolated. Inflammation in ulcerative colitis gut tissue decreased when the tissue was exposed to healthy liver cells. At the same time, genes and cellular pathways involved in metabolism and immune function became more active in both organs.
Adding two types of T cells to the system: CD4+ T regulatory cells and TH17 cells- quickly increased inflammation and recreated certain features of both IBD and autoimmune liver diseases.
Scientists next determined the potential role of molecules called short-chain fatty acids (SCFAs) in inflammatory disease. They found that adding SCFAs to the ulcerative colitis model greatly exacerbated inflammation throughout the liver and gut, but only if T cells were already present.
Martin Trapecar, an MIT postdoc and the lead author of the paper, said, “The hypothesis we formed, based on these studies, is that the role of short-chain fatty acids seems to depend on how much the adaptive immune system (which includes T cells) is involved.”
“That is, in the early stages of inflammation, when T cells are not heavily involved, SCFAs can help reduce inflammation. But when many effector T cells are recruited, SCFAs stimulate them to be even more inflammatory. This could be useful in cases of infection, to help the body to fend off invaders, but it can also accelerate autoimmune disorders.”
Linda Griffith, the School of Engineering Professor of Teaching Innovation, a professor of biological engineering and mechanical engineering, and the senior author of the study said, “We’ve shown that now you can start to attack some of these thorny, chronic inflammatory diseases by designing experiments in these organs on chips.”
Journal Reference:
- Gut-Liver Physiomimetics Reveal Paradoxical Modulation of IBD-Related Inflammation by Short-Chain Fatty Acids. DOI: 10.1016/j.cels.2020.02.008