Rotaviruses (RVs) are intestinal viruses that frequently cause severe diarrheal illness and largely reproduce in the small intestine. The following intestinal infection generally causes various levels of protective systemic and mucosal immune responses in humans and other animals.
The simian RV known as rhesus rotavirus (RRV) has been well-researched in mice and has previously been employed as a human RV vaccine.
Every year, norovirus causes hundreds of millions of cases of food poisoning and at least 50,000 deaths. However, there is no effective way to control it. Scientists have struggled to develop effective vaccines and drugs because the virus has proven challenging to study in the lab.
A new study from Washington University School of Medicine in St. Louis describes a novel approach to developing a norovirus vaccine by building on the highly effective vaccines for rotavirus. This unrelated virus also causes diarrhea.
The researchers developed an experimental rotavirus-norovirus combo vaccine by combining a key protein from norovirus with a harmless rotavirus strain. Mice given the experimental vaccine developed antibodies that neutralized both rotavirus and norovirus.
Senior author Siyuan Ding, an assistant professor of molecular microbiology, said, “Pretty much everyone has had norovirus at some point. You go out to eat, and the next thing you know, you’re vomiting and having diarrhea. You will recover, but it will be a rough three days or so. It can be deadly for kids in the developing world who don’t have access to clean water. The rotavirus vaccines work well, and global distribution systems are already set up for them. Based on that, we finally saw an opportunity to make some headway against norovirus.”
Before the first rotavirus vaccines were introduced in 2006, half a million children died yearly from rotavirus-caused diarrhea. The figure is now estimated to be around 200,000, which is still a significant improvement.
Four rotavirus vaccines are currently in use worldwide, but human norovirus has hampered scientific research for decades. All are live-virus vaccines, which means they are based on weakened forms of rotavirus capable of triggering an immune response but not making people sick.
Because it does not infect mice, rats, or other common laboratory animals, the types of experiments that led to the development of rotavirus vaccines are impossible to replicate with norovirus.
Ding and colleagues proposed using rotavirus to avoid the technical difficulties associated with working with norovirus. They used a laboratory rotavirus strain to simulate one of the approved vaccines.
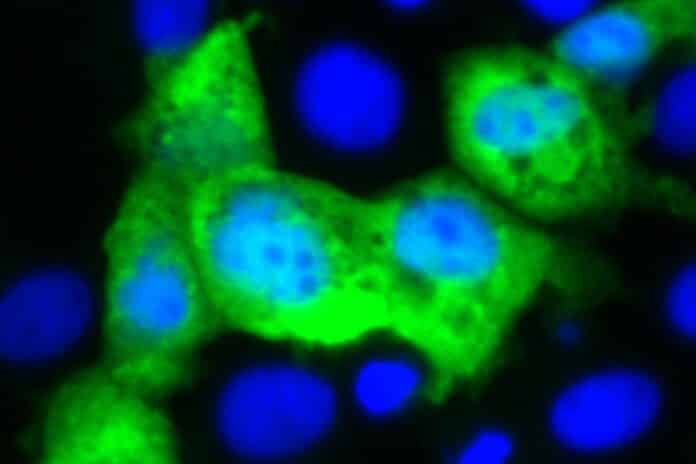
They inserted the gene for the protein that formed the outer surface of human norovirus into the genome of a rotavirus lab strain and gave the modified rotavirus to immunocompromised infant mice. They collected blood and fecal samples four, six, and eight weeks later. They gave the mice a booster shot nine weeks after the initial immunization and collected samples again a week later.
A strong antibody response was detected in the blood and intestines of nine of the eleven mice tested. Even better, some blood and intestine antibodies could neutralize both viruses in human “mini-gut” cultures in a dish. Organoids are cultures grown from human stem cells and replicate the surface of the human gut.
He said, “Traditionally, vaccine studies have focused on the antibody response in the blood because we understand that part of the immune response the best. But norovirus and rotavirus are gut viruses, so antibodies in the blood are less important than the ones in the intestines in terms of fighting off these viruses. The fact that we saw a strong antibody response in the intestines is a good sign.”
The next step is to demonstrate that animals immunized with the experimental vaccine are less likely to become ill or die from norovirus. Ding is currently conducting such experiments.
He said, “There are a lot of intestinal pathogens out there for which we don’t have good treatments or vaccines. We could put a gene from any organism that infects the intestinal tract into the rotavirus vaccine to create a bivalent vaccine. Of course, we’d have to find the right targets to produce a good immune response, but the principle is simple.”
This study describes a novel approach to vaccine development for a variety of troublesome organisms that cause diarrhea, particularly in resource-limited countries where many of these infections occur.
The researcher continued, “As basic scientists, we rarely get the chance to actually move something forward into the clinic. We study what the virus does and how the host responds at a basic level. This is a rare opportunity for our work to affect human health directly and improve people’s lives.”
Journal Reference:
- Kawagishi, Ding, etal. Mucosal and systemic neutralizing antibodies to norovirus induced in infant mice orally inoculated with recombinant rotaviruses. Proceedings of the National Academy of Sciences. DOI: 10.1073/pnas.2214421120