MIT scientists have developed a system to measure the patient’s pain level by detecting their brain activity. The system is expected to help doctors diagnose and trat pain unconscious and noncommunicative patients, which could reduce the risk of chronic pain that can occur after surgery.
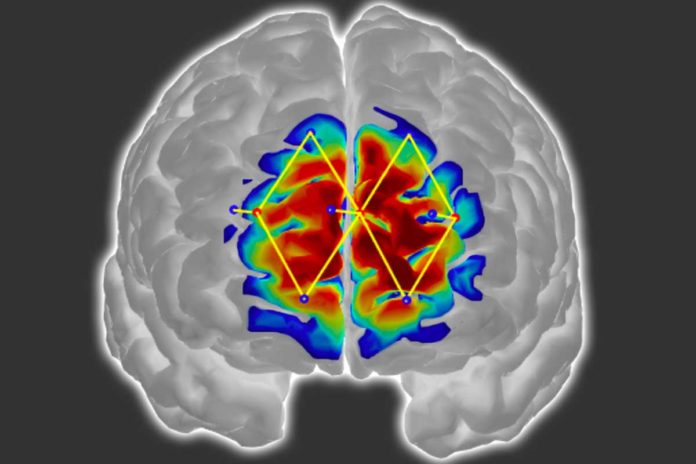
To develop the system, scinetists used functional near infrared spectroscopy (fNIRS), a technique that offers a relatively non-invasive, safe, portable, and low-cost method of indirect and direct monitoring of brain activity. By measuring changes in near-infrared light, it allows researchers to monitor blood flow in the front part of the brain.
Then by measuring brain signals, scientists developed personalized machine-learning models to recognize patterns of oxygenated hemoglobin levels related with pain responses. When the sensors are set up, the models can distinguish whether a patient is experiencing pain with around 87 percent precision.
Daniel Lopez-Martinez, a PhD student in the Harvard-MIT Program in Health Sciences and Technology and a researcher at the MIT Media Lab said, “The way we measure pain hasn’t changed over the years. If we don’t have metrics for how much pain someone experiences, treating pain and running clinical trials becomes challenging. The motivation is to quantify pain in an objective manner that doesn’t require the cooperation of the patient, such as when a patient is unconscious during surgery.”
Scientists trained andtested the model on a labeled pain-processing dataset they collected from 43 male participants. Each participant wore the researchers’ fNIRS device and was randomly exposed to an innocuous sensation and then about a dozen shocks to their thumb at two different pain intensities, measured on a scale of 1-10: a low level (about a 3/10) or high level (about 7/10).
Those two intensities were determined with pretests: The participants self-reported the low level as being only strongly aware of the shock without pain, and the high level as the maximum pain they could tolerate.
In training, the model extracted dozens of features from the signals related to how much oxygenated and deoxygenated hemoglobin was present, as well as how quickly the oxygenated hemoglobin levels rose. Those two metrics — quantity and speed — give a clearer picture of a patient’s experience of pain at the different intensities.
Importantly, the model also automatically generates “personalized” submodels that extract high-resolution features from individual patient subpopulations. Traditionally, in machine learning, one model learns classifications — “pain” or “no pain” — based on average responses of the entire patient population. But that generalized approach can reduce accuracy, especially with diverse patient populations. The researchers’ model instead trains on the entire population but simultaneously identifies shared characteristics among subpopulations within the larger dataset.
When scientists compared personalized and traditional model, the personalized model outperformed the traditional model by about 20 percent, reaching about 87 percent accuracy.
Lopez-Martinez said, “Because we are able to detect pain with this high accuracy, using only a few sensors on the forehead, we have a solid basis for bringing this technology to a real-world clinical setting.”