Treating type-1 diabetes by transplanting islet cells becomes a trend but proven challenging. One impediment is that once the islets are transplanted, they will kick the bucket in the event that they don’t get a sufficient supply of oxygen.
Presently, scientists at MIT, working with an organization called Beta-O2 Technologies, have created and tried an implantable gadget that outfits islet cells with their own supply of oxygen, by means of a chamber that can be recharged like clockwork.
The approach keeps islets functional and thus reduce the ability of the implants to provoke an immune response. The trial of these inserts in rats demonstrated that about 90 percent of the islets stayed reasonable for a while, and the majority of the rats kept up ordinary blood glucose levels all through that time.
One reason the transplanted islets fizzled is that they were assaulted by the patients’ resistant frameworks. To ensure the transplanted cells, specialists have started creating inserts in which the islets are epitomized in a material, for example, a polymer. Nonetheless, a residual test is ensuring that the islets get enough oxygen, Colton says.
In a sound pancreas, all islet cells come into contact with vessels, enabling them to get oxygen-rich blood, at an oxygen fractional weight of around 100 millimeters of mercury (mm Hg). (Halfway weight is a measure of the grouping of an individual gas inside a blend of gases). At the point when specialists initially endeavored to transplant islets into diabetic patients, a considerable lot of the cells did not have any immediate contact with vessels, so their oxygen supply was too low.
Past research in Colton’s lab found that the external surface of islets should be presented to no less than 50 mm Hg of oxygen to stay feasible and create insulin ordinarily. Through a progression of tests, the MIT group, working with scientists at Beta-O2 Technologies, decided the working states of the gadget required for islets to remain alive and work for drawn-out stretches of time while amassed in a minimal frame sufficiently little to be embedded in human patients.
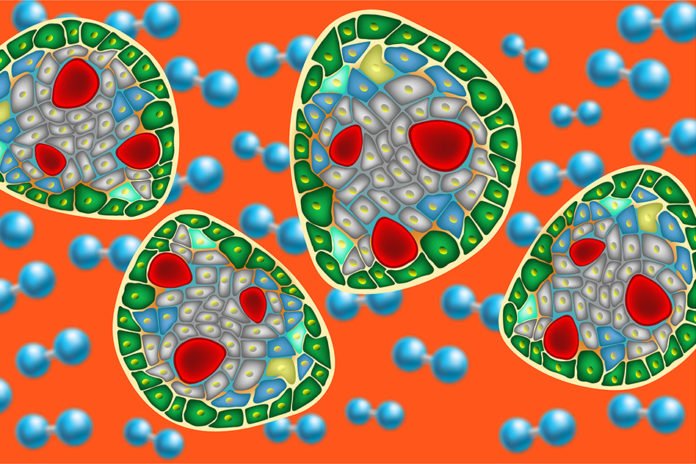
In this newly developed device, islets are epitomized in a chunk of alginate, a polysaccharide delivered by algae, around 600 microns thick. A membrane on one side of chunk keeps out immune cells and extensive proteins, however, permit insulin, supplements, and oxygen through. Beneath the chunk is the gas chamber, around 5 millimeters thick, which conveys barometrical gases, for example, nitrogen and carbon dioxide notwithstanding oxygen. Oxygen streams from the chamber, over the semipermeable layer, and into the islets implanted in the alginate section.
As oxygen diffuses through the section, it is progressively devoured, so the oxygen incomplete weight persistently drops. To guarantee that the halfway weight stays no less than 50 mm Hg for 24 hours, the analysts found that they expected in the first place an oxygen fractional weight of 500 mm Hg in the gas chamber.
Following 24 hours, the oxygen supply is recharged through a port — a gadget embedded under the skin and associated with a catheter that prompts the typified islets, which are likewise embedded under the skin.
During tests, scientists showed that nearly 90 percent of the islets survived the entire transplant period, which ranged from 11 weeks to eight months. They also found that most of these animals’ blood sugar levels remained normal while the devices were implanted, then rebounded to diabetic levels after they were removed.
And as most of the islet cells remain functional, they are less likely to provoke an immune response. When cells die, they break down, and the resulting fragments of protein and DNA are more likely to attract the attention of the immune system.
Clark Colton, an MIT professor of chemical engineering and the senior author of the study said, “By keeping the cells alive, you minimize the immune response.”
James Shapiro, a professor of surgery, medicine, and surgical oncology at the University of Alberta said, “This kind of device can protect the cells from immune attack and deliver oxygen in a way that allows more cells to survive. This would allow islet cells to be transplanted in patients without antirejection drugs, which would dramatically improve the safety of what we’re doing today with islet cell transplantation.”
Researchers at Beta-O2 Technologies are now working on new versions of the device in which an oxygen storage chamber is implanted below the skin, separate from the islets. This version would only need to be replenished once a week, which could be more appealing to patients.
Yoav Evron of Beta-O2 Technologies is the lead author of the study, which appears in the April 25 issue of Scientific Reports.