Infertility impacts 10% of the U.S. populace, and its rates have expanded in past decades. Numerous types of infertility can be dealt with using strategies that combine egg and sperm outside the body, for example, in vitro fertilization (IVF) and intracytoplasmic sperm infusion.
Be that as it may, for individuals whose bodies don’t produce eggs or sperm—because of chemotherapy, radiation, genetics, or other unexplained causes—those treatments aren’t an alternative except if a donor gives the eggs or sperm.
Amander Clark, the study’s lead author, a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA, said, “With donated eggs and sperm, the child is not genetically related to one or both parents. To treat patients who want a child who is genetically related, we need to understand how to make germ cells from stem cells, and then how to coax those germ cells into eggs or sperm.”
In a new study, scientists studied how and when the precursors to eggs and sperm are formed during development could help pave the way for generating egg and sperm cells in the lab to treat infertility.
The study particularly highlights how human stem cells evolve into germ cells, the precursors for egg and sperm cells.
Clark said, “Right now, if your body doesn’t make germ cells, then there’s no option for having a child that’s biologically related to you. What we want to do is use stem cells to be able to generate germ cells outside the human body so that this kind of infertility can be overcome.”
In developing male and female embryos, a subset of pluripotent stem cells—cells that can turn out to be about each type of cell in the body—become germ cells that will later produce eggs or sperm. In past study, scientists demonstrated the capability to make similar stem cells in a lab, called induced pluripotent stem cells, or iPS cells, from a person’s skin or blood cells.
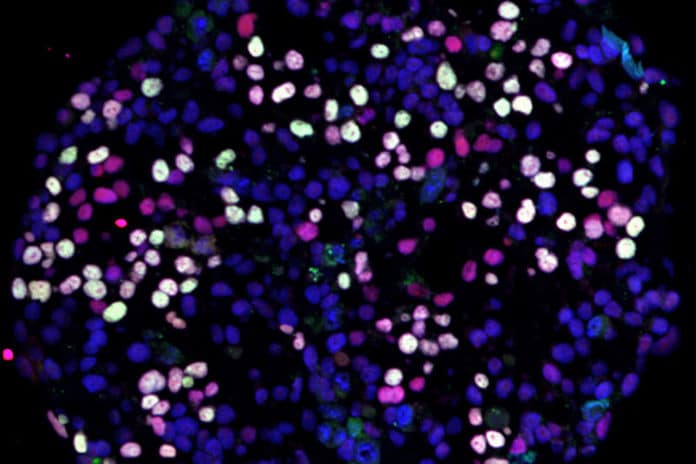
Scientists used technology that enabled them to quantify the active genes in more than 100,000 embryonic stem cells and iPS cells as they generated germ cells. New algorithms have also been developed to analyze the massive amounts of data.
Their experiment unveiled the duration when germ cells likely to form: They first become distinct from other cells of the body between 24 and 48 hours after stem cells start differentiating into cell types that will ultimately make up all the specialized cells in the adult body.
The study also revealed that the germ cells come from two different populations of stem cells—amnion cells and gastrulating cells.
Comparing the germ cells derived from embryonic stem cells with those derived from iPS cells in the lab, scientists detected the patterns by which genes were activated were nearly identical.
Clark said, “This tells us that the approach we’re using to begin the process of making germ cells is on the right track. Now we’re poised to take the next step of combining these cells with ovary or testis cells.”
The following stage is essential because molecular signals from the ovary or testis tissue are what signal germ cells to develop into eggs and sperm.
If the methodology was to be fused into a future treatment for infertility, researchers may, in the end, have the option to utilize a patient’s skin cells to form stem cells that can be influenced into both germ cells and ovarian or testis tissue—and those cell types may have the option to be utilized to produce an individual’s eggs or sperm in the lab.
Clark said, “We’re going in the right direction, but it will take a lot of innovations to solve infertility related to the loss of germ cells.”
The study, published in the journal Cell Reports.