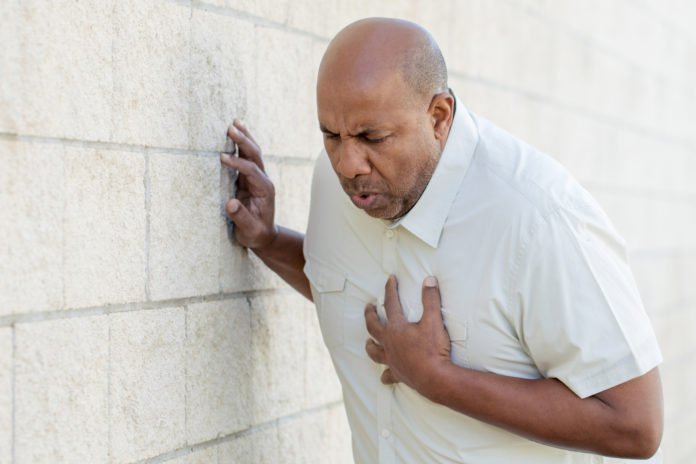
In the United States, heart disease is the leading cause of death, and stroke is the fifth-leading cause. A major contributor to these cardiovascular diseases is clogged blood vessels (atherosclerosis), which result from the buildup of fatty deposits or plaque.
Treatment for obstructed veins regularly incorporates angioplasty. In this methodology, the specialist embeds a little, medicinal inflatable into the harmed veins, and after that expands and evacuates it. Little tubes, or stents, additionally might be utilized to hold open the veins. To keep additionally harm from happening, patients regularly take numerous blood thinners, for example, clopidogrel and ibuprofen, after stent situation.
Many previous studies have suggested that clopidogrel is less effective in patients with mutations in a specific gene, called CYP2C19 than in patients without the mutations. Whether genetic testing can help guide treatment in clinical practice, however, has remained unclear.
In a new study by the American Heart Association, scientists suggest that using genetic testing to illuminate which blood more slender to utilize following a methodology to open limited veins brought about essentially fewer entanglements among patients.
The results also showed that genetic testing for CYP2C19 mutations could be used to guide blood-thinner treatment after stent placement. Patients with the changes who got one of two clopidogrel choices contrasted with clopidogrel were in excess of three times less inclined to bite the dust or show some kindness assault, stroke or other significant confusions a year after treatment.
Study participants included 1,193 patients at the University of North Carolina Cardiac Catheterization Laboratory who received stent placement between July 1, 2012, and June 30, 2014. Their average age was 63 years and more than two-thirds were male. Most were white, 21 percent were black, and 1 percent was Asian. Patients identified as high risk, due to decreased blood flow to the heart, received the genetic testing. Follow up was 12 months.
The study has several limitations. For one, the investigators collected information after treatment, so they could not definitively say whether blood-thinner choice and the results of genetic testing caused better patient outcomes. Another limitation includes the use of a single hospital, which may not be applicable to different settings.
In particular, significant entanglements happened among 27 percent of clopidogrel patients with the hereditary transformations, contrasted with 8 percent of patients with the changes who got the elective meds.
These discoveries are like those of a prior, multicenter contemplate that found the danger of a noteworthy cardiovascular occasion dramatically increased in patients with the hereditary transformations who took clopidogrel.
Craig R. Lee, Pharm.D., Ph.D., F.A.H.A., associate professor of pharmacy at the University of North Carolina at Chapel Hill Eshelman School of Pharmacy said, “Using an algorithm based on genetic testing to guide treatment is sustainable and associated with better clinical outcomes in a real-world clinical practice, although it is difficult to consistently maintain. Clinicians need to be aware of the increased risk of major adverse cardiovascular events associated with the use of clopidogrel in patients receiving stents who carry either one or two copies of the mutation.”
George “Rick” Stouffer, III, M.D., F.A.H.A., chief of cardiology said, “We are using CYP2C19 genetic testing on a daily basis at our institution to help decide in a timely manner which drug to prescribe.”
The study is published online in Circulation: Genomic and Precision Medicine.