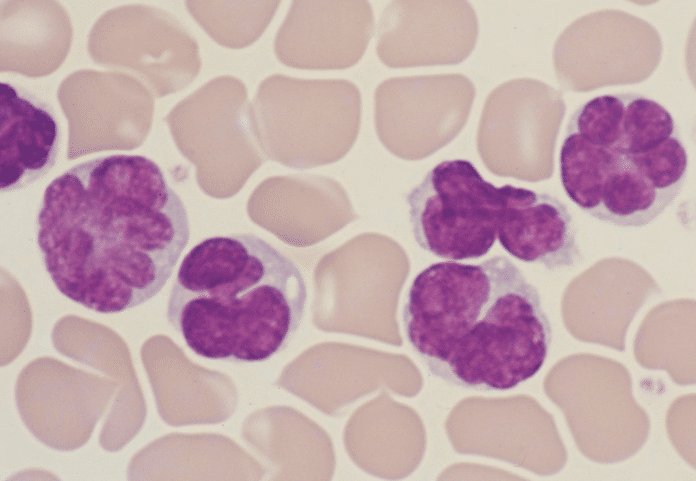
T-cell leukemia/lymphoma (ATL) is rare cancer, develops in around five percent of people infected with the HTLV-1 virus. The virus infects T-cells and transforms them into leukemia cells. However, it remains elusive how this transformation occurs.
In collaboration with Kumamoto University in Japan, scientists from the Imperial College London have determined how the virus over-activates T-cells and causes them to turn cancerous.
They found that the virus hijacks the activation machinery of T-cells, causing them to persist at a high level of activation, gradually becoming malignant.
Scientists studied over 87,000 T-cells from virus-free donors, healthy carriers of the virus, and patients with ATL. They sequenced RNA from these cells to determine how the virus and T-cells interacted.
In people with ATL, they found that HTLV-1 made infected T-cells highly activated and over-reactive. This causes T-cells to over-produce proteins that keep them proliferating and help them avoid other parts of the immune system that would usually remove rogue cells.
According to scientists, these changes made the overactive T-cells more vulnerable to DNA damage, such as chemical agents or radiation, accelerating their transition to a cancerous state.
Co-lead researcher Professor Yorifumi Satou from Kumamoto University is a virologist studying HTLV-1. He said: “While only a small percentage of people with HTLV-1 viral infections go on to develop adult T-cell leukemia/lymphoma, there are estimated to be around five to ten million carriers of the virus worldwide, and in some areas, it is endemic – for example, there are around one million cases in Japan.”
Co-lead researcher Dr. Masahiro Ono, from the Department of Life Sciences at Imperial, is an immunologist and cell biologist who brought his knowledge of T-cells to the project. He said: “There is, therefore, a great need to understand how the virus turns our T-cells against us in the progression to cancer. Our work highlights a key mechanism for this change and provides us with new directions to search for ways to interfere with the process, potentially preventing cancer from developing.”
“Further study of the processes involved will lay the foundations for potential new treatment options. For example, the chronic activation of T-cells could be halted by molecules that block signaling pathways that tell the cells to activate. Alternatively, treatments could target the proteins the activated T-cells create to help them proliferate.”
The team’s results published today in The Journal of Clinical Investigation.