Red blood cells are an essential element of blood. Their job is to transport oxygen to the body’s tissues in exchange for carbon dioxide, which is carried to and eliminated by the lungs. RBCs also aid the body in fighting against infections by capturing pathogens on their surfaces, neutralizing them, and presenting them to immune cells in the spleen and liver.
Now, scientists at Harvard’s Wyss Institute for Biologically Inspired Engineering and John A. Paulson School of Engineering and Applied Sciences (SEAS) took inspiration from this innate ability. They developed a platform technology that uses red blood cells to deliver antigens to antigen-presenting cells (APCs) in the spleen, generating an immune response.
The technology called Erythrocyte-Driven Immune Targeting (EDIT) slowed the growth of cancerous tumors in mice. It is also expected to be used as a biocompatible adjuvant for a variety of vaccines.
To develop this technology, scientists first needed to comprehend how to get antigens to stick to red blood cells strongly enough to resist shearing off and reach the spleen.
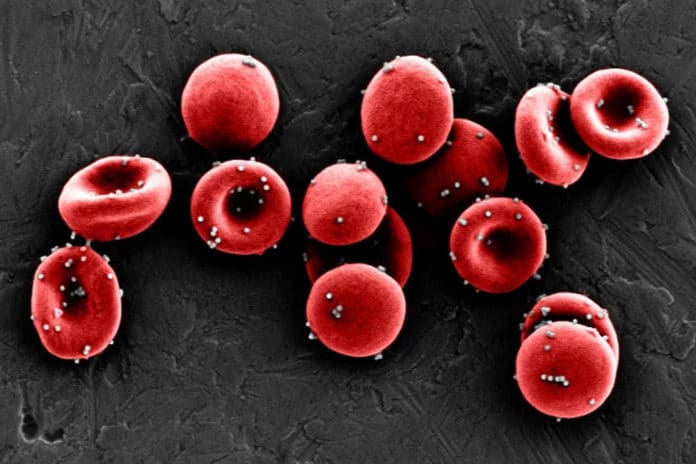
They coated polystyrene nanoparticles with ovalbumin, an antigenic protein known to cause a mild immune response, then incubated them with mouse red blood cells. The ratio of 300 nanoparticles per blood cell resulted in the greatest number of nanoparticles bound to the cells, retention of about 80 percent of the nanoparticles when the cells were exposed to the shear stress found in lung capillaries, and moderate expression of a lipid molecule called phosphatidylserine (PS) on the cells’ membranes.
Anvay Ukidve, a graduate student in the Mitragotri lab and co-first author of the paper said, “A high level of PS on red blood cells is essentially an ‘eat me’ signal that causes them to be digested by the spleen when they are stressed or damaged, which we wanted to avoid. We hoped that a lower amount of PS would instead temporarily signal ‘check me out’ to the spleen’s APCs, which would then take up the red blood cells’ antigen-coated nanoparticles without the cells themselves getting destroyed.”
To test that speculation, the group infused red blood cells coated with their nanoparticles into mice, then followed where they gathered in their bodies. Twenty minutes after infusion, more than 99 percent of the nanoparticles had been cleared from the animals’ blood, and more nanoparticles were available in their spleens than their lungs.
The higher nanoparticle accumulation in the spleen persisted for up to 24 hours, and the number of EDIT red blood cells in the circulation remained unchanged, showing that the red blood cells had successfully delivered their cargoes to the spleen without being destroyed.
Once confirming that nanoparticles were successfully delivered to the spleen in vivo, scientists later assessed whether the antigens on the nanoparticles’ surfaces induced an immune response.
Mice were injected with EDIT once a week for three weeks, and then their spleen cells were analyzed. Treated mice displayed eight-fold and 2.2-fold more T cells displaying the delivered ovalbumin antigen than mice that were given “free” nanoparticles or were untreated, respectively. Mice treated with EDIT also produced more antibodies against ovalbumin in their blood than either of the other groups of mice.
Scientists repeated their three-week prophylactic injection of EDIT into mice to check whether this technology potentially prevents or treats disease. They also inoculated them with lymphoma cells that expressed ovalbumin on their surfaces.
The mice that received EDIT had about three-fold slower tumor growth compared with the control group and the group that received free nanoparticles and had lower numbers of viable cancerous cells. This outcome significantly increased the window of time during which the tumor could be treated before the mice succumbed to the disease.
Zongmin Zhao, a co-first author of the paper, said, “EDIT essentially is an adjuvant-free vaccine platform. Part of the reason why vaccine development today takes so long is that foreign adjuvants delivered along with an antigen have to go through a full clinical safety trial for each new vaccine. Red blood cells have been safely transfused into patients for centuries, and their ability to enhance immune responses could make them a safe alternative to foreign adjuvants, increasing the efficacy of vaccines and speed of vaccine creation.”
Additional authors of the paper include Vinu Krishnan, Daniel C. Pan, Yongsheng Gao, and Abhirup Mandal from the Wyss Institute and SEAS; Alexandra Fehnel from SEAS, and Vladimir Muzykantov from the Perelman School of Medicine at the University of Pennsylvania. This research was supported by the Wyss Institute at Harvard University and the National Institutes of Health under grant # 1R01HL143806-01.
Journal Reference:
- Anvay Ukidve el al., “Erythrocyte-driven immunization via biomimicry of their natural antigen-presenting function,” PNAS (2020). DOI: 10.1073/pnas.2002880117