Insulin therapy in the setting of type 1 and advanced type 2 diabetes is complicated by an increased risk of hypoglycemia, a condition caused by a very low level of blood sugar (glucose), your body’s main energy source.
Sometimes, the condition may even lead to seizures, coma, and in extreme cases, death. Thus, as a safety check, the UCLA-led team has developed a type of smart insulin, called i-insulin that can prevent blood sugar levels from dipping too low. This smart insulin is nothing but an insulin-facilitated glucose transporter (Glut) inhibitor conjugate, in which the insulin molecule is rendered glucose-responsive via conjugation to an inhibitor of Glut.
To create this smart insulin, scientists added an additional molecule called a glucose transporter inhibitor to insulin to create the new smart insulin. The inhibitor chemically blocks the glucose transporter molecule that has come to the surface.
Its presence doesn’t block all glucose from entering, nor does it permanently obstruct the transporter molecules. Rather, it’s a piece of a dynamic procedure that relies upon what number of inhibitor and glucose molecules are present.
It works by letting the glucose get into the cell, but the added inhibitor molecule prevents too much from going in when blood sugar is normal. This keeps blood sugar at normal levels and reduces the risk of hypoglycemia. In addition, it responds rapidly to high glucose levels. For example, after a meal, when glucose levels climb, the insulin level in the bloodstream also quickly increases, which helps normalize the glucose level.
Scientists tested smart insulin on mice with Type 1 diabetes. The i-insulin controlled glucose levels within the normal range for up to 10 hours after the first injection. A second injection three hours later extended the protection from hypoglycemia.
Dr. John Buse, a professor and director of the Diabetes Care Center at the University of North Carolina School of Medicine said, “The next step is to further evaluate the long-term biocompatibility of the modified insulin system in an animal model before determining whether to move to clinical trials. The vision, if realized, would be one of the most exciting advances in diabetes care.”
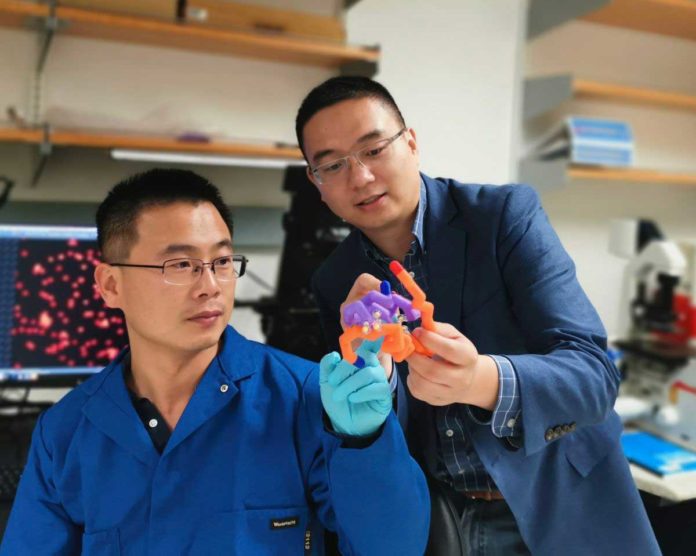
Zhen Gu, a professor of bioengineering at the UCLA Samueli School of Engineering said, “The new insulin has the potential to be optimized for response times and how long it could last in the body before another dose would be required. And it could be delivered in other methods, such as a skin patch with tiny needles, or in pills.”
The study’s other lead author is Jicheng Yu, chief scientific officer of pharmaceutical company Zenomics and a former doctoral student in Gu’s lab.
The study was published in the Proceedings of the National Academy of Sciences.