Dysregulation of the prefrontal cortex’s input to the nucleus accumbens (NAc) contributes to cue-induced opioid seeking.
Changes in the activity of pyramidal neurons, which lead to drug-seeking in a preclinical model of opioid use disorder, have been detected by a team of neuroscientists at the Medical University of South Carolina (MUSC).
When heroin was no longer available, these neurons became more excitable. They returned to normal by inhibiting the enzyme protein kinase A (PKA). Inhibiting this enzyme lowered opioid-seeking behavior as well.
The risk of opioid overdose can increase upon return to drug seeking and use, or relapse, after a period of not using the drug or abstinence.
Kokane said, “Prevention of return to use is the key to the successful development of effective treatments for substance use disorders. After decades of research on opioid use disorder, three FDA-approved drugs exist, but they only reduce the severity of detoxification symptoms and don’t stop return to use. So, there is a definite need for more treatment options.”
He also said. “Currently, we lack a comprehensive understanding of the effects of opioids, like heroin, on the neurons that drive return to use. A better understanding of these changes may lead to additional treatment options. The changes in the brain of someone recovering from substance use disorder drive a return to use when environmental drug cues become overwhelming, but the exact types of changes that occur have not been fully studied.”
The McGinty Lab at MUSC identified specific types of pyramidal neurons contributing to relapse.
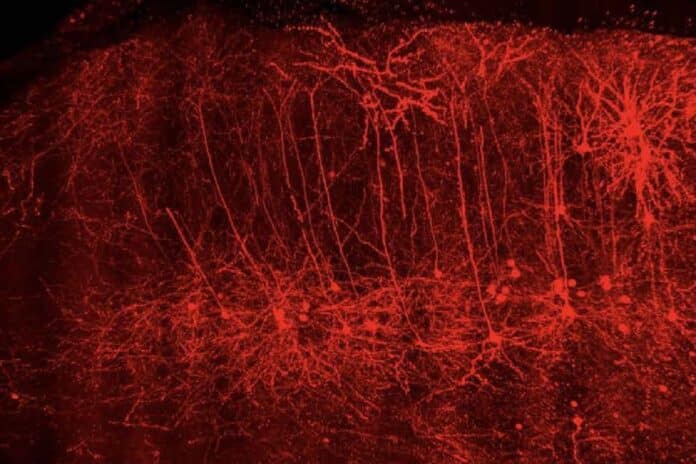
They discovered that these neurons in a specific brain region, the prelimbic prefrontal cortex, undergo molecular and functional changes during heroin abstinence, which disrupt their function.
The researchers show in this preclinical study that restoring normal function to these neurons by inhibiting a key enzyme during heroin abstinence can prevent drug seeking in a rodent model.
These disorders are defined in part by the continued use of substances despite negative consequences, as well as periods of abstinence followed by a return to use or relapse. One type, cue-induced relapse, can occur when someone with a substance use disorder encounters a “cue” or “trigger” that may lead them to crave the use of a drug. For example, someone with an alcohol use disorder may crave a drink when they hear the pop of champagne.
He said, “These overwhelming cravings may lead those with opioid use disorders to return to use, even if they do not want to.”
McGinty said, “The challenges with compulsive drug use are the loss of the ability to decide between different behavioral options and the lack of resistance to environmental stimuli that remind you of taking an opioid like heroin.”
Changes in several brain regions are responsible for cue-induced relapse and make it difficult for a person with substance use disorder to control drug cravings. In this study, Kokane and the McGinty Lab focused on two regions: the nucleus accumbens and the prelimbic cortex.
The researcher explained, “The nucleus accumbens is a brain area that receives input from the prelimbic cortex and from dopamine-releasing pathways that cause the desire to take the substance again that is associated with all addictive drugs, including opioids.”
During abstinence, aberrant functioning of these pathways is a major contributor to cue-induced relapse.
Generally, the prelimbic cortex and other cortical regions are responsible for deciding whether to act on a feeling or desire. Through its connections with the nucleus accumbens, the prelimbic cortex either motivates us to stop acting or pushes us to work.
Kokane said, “Our findings suggest that research should be geared toward developing pharmacotherapies that specifically target functional changes that develop during heroin abstinence in particular types of neurons, like those we identified in the prelimbic cortex.”
The nucleus accumbens is a brain area that receives input from the prelimbic cortex and dopamine-releasing pathways that cause the desire to take the substance again. During abstinence, aberrant functioning of these pathways is a major contributor to cue-induced relapse.
The prelimbic cortex is responsible for deciding whether to act on a feeling or desire. Research should be geared toward developing pharmacotherapies targeting functional changes that develop during heroin abstinence in particular types of neurons, like those we identified in the prelimbic cortex.
Using a rodent model, the MUSC team found that neurons connecting the prelimbic cortex to the nucleus accumbens increase their activity during abstinence from heroin.
This increased activity may help the nucleus accumbens to drive relapse, often despite negative social and psychological consequences. The MUSC study also discovered that an enzyme, PKA, is more active during heroin abstinence.
By blocking PKA, the researchers discovered one way to restore control to the prelimbic cortex during opioid abstinence in a rodent model, leading to a decrease in cue-induced relapse and better behavioral control.
McGinty said, “It is important to realize that the brain is constantly adapting to the environment and that the changes we have documented in the prefrontal cortex during heroin abstinence, while persistent, are not necessarily permanent and are subject to reversal.”
Journal Reference:
- Saurabh S. Kokane, Robert D. Cole, et al. Increased Excitability and Synaptic Plasticity of Drd1- and Drd2- expressing Prelimbic Neurons Projecting to the Nucleus Accumbens after Heroin Abstinence are Reversed by Cue-induced Relapse and Protein Kinase A Inhibition. Journal of Neuroscience. DOI: 10.1523/JNEUROSCI.0108-23.2023