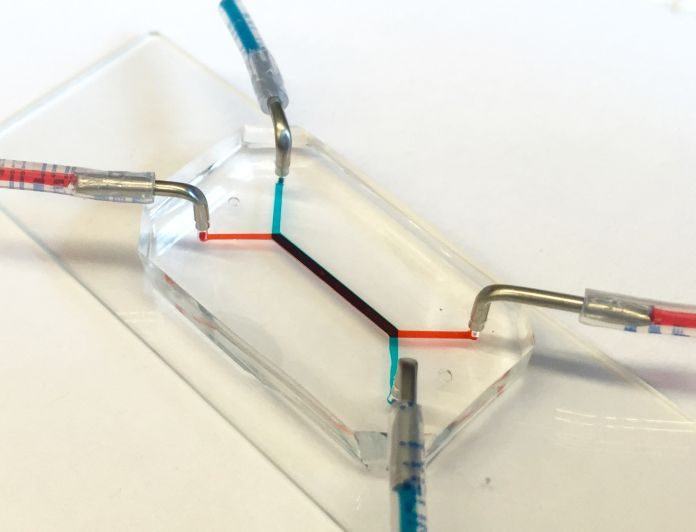
Scientists from the University of Pennsylvania have developed first ever placenta-on-a-chip. It is able to design the transport of nutrients against the placental barrier. This device has a size of similar to a flash drive that consists of two layers made from human cells, design interface between mother and fetus. On the other side of these layers, microfluidic channels allow scientists to analyze how molecules are transported through, or are blocked by, that interface.
This chip provides a unique ability to act and analyze the function of the human brain. It performs in such way that is not possible with conventional tools.
How was placenta-on-a-chip made?
The placenta-on-a-chip is silicon device. There are two parallel microfluidic channels, that are disconnected by a porous membrane. The trophoblast cells are grown at the one side of these porous. These trophoblast cells are generally found in the placental interface with blood material. Whereas, endothelial cells are grown on the other side, which is found on inside fetal blood vessels. The layers of both cells act as a placental barrier, the protector between the maternal and fetal circulatory systems.
This barrier resolves complete transport between mother and fetal. Transport is one of the essential function of the placemental barrier. So, it is necessary to perform that function.
Previously, in 2013, Dan Huh, had conducted a study on creating a microfluidic device for culturing trophoblast cells and fetal endothelial cells. But, this model did not have the ability to form physiological placental tissue and precisely imitate transport function of the placental barrier.
But, to overcome this deficiency, scientists now discover syncytialization process. In this process, those two layers of cell grow continuously and evolves while under the chip.
Huh said, “The placental cells change over the course of pregnancy. During pregnancy, the placental trophoblast cells actually fuse with one another to create interesting tissue called syncytium. The barrier also becomes thinner as the pregnancy progresses, and with our new model we’re able to reproduce this change.”
This is an essential process because it affects placental transport. Researchers showed glucose transfer rates against syncytialized barrier to authorize this new model.
Huh said, “The placenta is arguably the least understood organ in the human body. There are more remains to be learned about how transport between mother and fetus works at the tissue, cellular and molecular levels. An isolated whole organ is a not ideal platform for these types of mechanistic studies.”
Cassidy Blundell, a graduate student in the Huh lab, said, “Above the deficiency of samples, there’s a limited lifespan of how long the tissue remains viable. It may be for only a few hours after delivery, and the system that is used to perfuse the tissue and perform transport studies is complex.”
Researchers hope that they will influence their model to discover the potential of organ-on-a-chip technology as a new strategy. They think that it will be used to innovate basic and translational research in reproductive biology and medicine.