The DNA in our cells is powerless to harm caused by outer factors, for example, daylight or smoking, or inward factors including our hereditary qualities. One type of harm is when the two strands of the DNA double helix break – this can prompt cell passing, so cells have different repair systems to settle the harm.
The least complex component for repairing DNA breaks is known as ‘non-homologous end-joining’ (NHEJ). This component basically ‘sticks together’ the broken DNA strands, yet it is imperfect and can delete the segments of DNA.
A more exact repair mechanism is ‘homologous recombination’ (HR). This component utilizes a duplicate of our DNA as a source to fill in any missing gaps. In any case, NHEJ and HR work in rivalry against each other: if the balance is tipped for HR, at that point cells will utilize this system to repair the DNA harm.
Among the proteins engaged with HR is BRCA1. Be that as it may, a few people convey a terrible BRCA1 change, which makes them more susceptible to cancer.
Scientists at the University of Cambridge discovered a protein complex that may explain the reason behind why some cancer patients develop resistance to their medication.
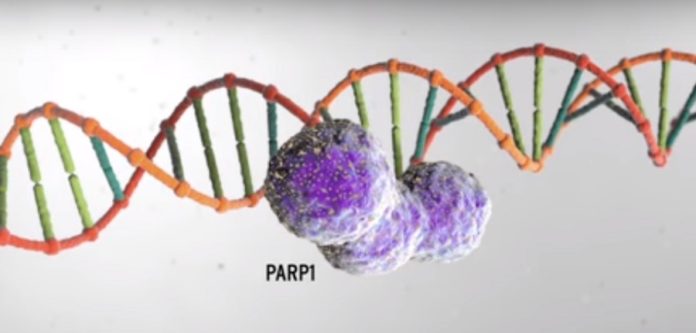
Scientists particularly identified patients who were treated with revolutionary new anti-cancer drugs known as PARP inhibitors develop resistance to their medication. They demonstrated that Shieldin, a component of the shieldin complex, which plays an important role in repair of DNA double-stranded breaks (DSBs).
To understand why patients who take PARP inhibitors develop resistance to the drugs, scientists used cutting-edge CRISPR-Cas 9 gene-editing techniques to screen breast cancer cells with the BRCA1 mutation and identify which genes drive resistance.
They distinguished two genes that create a protein complex currently alluded to as Shieldin. From this they could demonstrate that Shieldin assumes an imperative part in NHEJ, binding at the site of the broken strands of DNA. It is this complex that gives off an impression of being the way to patients reacting to PARP inhibitors.
The balancing act between NHEJ and HR should mean that the cells of people with the BRCA1 mutation cannot perform homologous recombination – hence PARP inhibitors are able to kill the cells. But when Shieldin levels are depleted – which may arise from spontaneous mutations in tumour cells – the balance changes and the patient’s tumour cells regain the ability to perform homologous recombination – and hence, PARP inhibitors are no longer effective.
Professor Jackson, whose group led the research, said: “There is a balancing act within our cells – a tug of war between proteins such as BRCA1 and Shieldin. Who wins determines whether the cell carries out error-free, albeit slower DNA repair, or faster, error-prone repair.”
The study’s lead author, Wellcome Clinical Fellow Dr Harveer Dev, explained: “In BRCA1 mutated cells, it appears as though the persistence of the Shieldin complex at DNA breaks renders these cells sensitive to PARP inhibitors. This explains why these drugs are normally effective in patients with BRCA1 mutations. But when Shieldin levels are low, patients can canngs. l Biology in July 2018..m stab.mplex.chosen is determined by a delicate balance between etings. l Biology in July 2018. develop resistance to these drugs.”
Professor Jackson concluded: “As we improve our understanding of these DNA repair networks and how they interact, we should be able to better predict the responsiveness of an individual patient’s tumor to specific therapies like PARP inhibitors, and ultimately personalize cancer therapy to achieve the maximum benefit.”
Professor Jackson concluded: “As we improve our understanding of these DNA repair networks and how they interact, we should be able to better predict the responsiveness of an individual patient’s tumor to specific therapies like PARP inhibitors, and ultimately personalize cancer therapy to achieve the maximum benefit.”
The study is published in Nature Cells Biology.