Powerhouses, called mitochondria, which provide fuel for our cells, start to fragment, likely as one of the first steps in the kidney cell damage and death that often result from an acute kidney injury.
Now, for the first ever time, scientists have described the body’s regular mechanism for briefly securing the powerhouses of kidney cells when damage or ailment implies they aren’t getting enough blood or oxygen. They precisely described the natural mitochondrial protection pathway.
According to scientists, the pathway is a logical therapeutic target for treating acute kidney injury.
Dr. Zheng Dong at Augusta University said, “We know there is a natural protective mechanism. Maybe we need to upregulate it.”
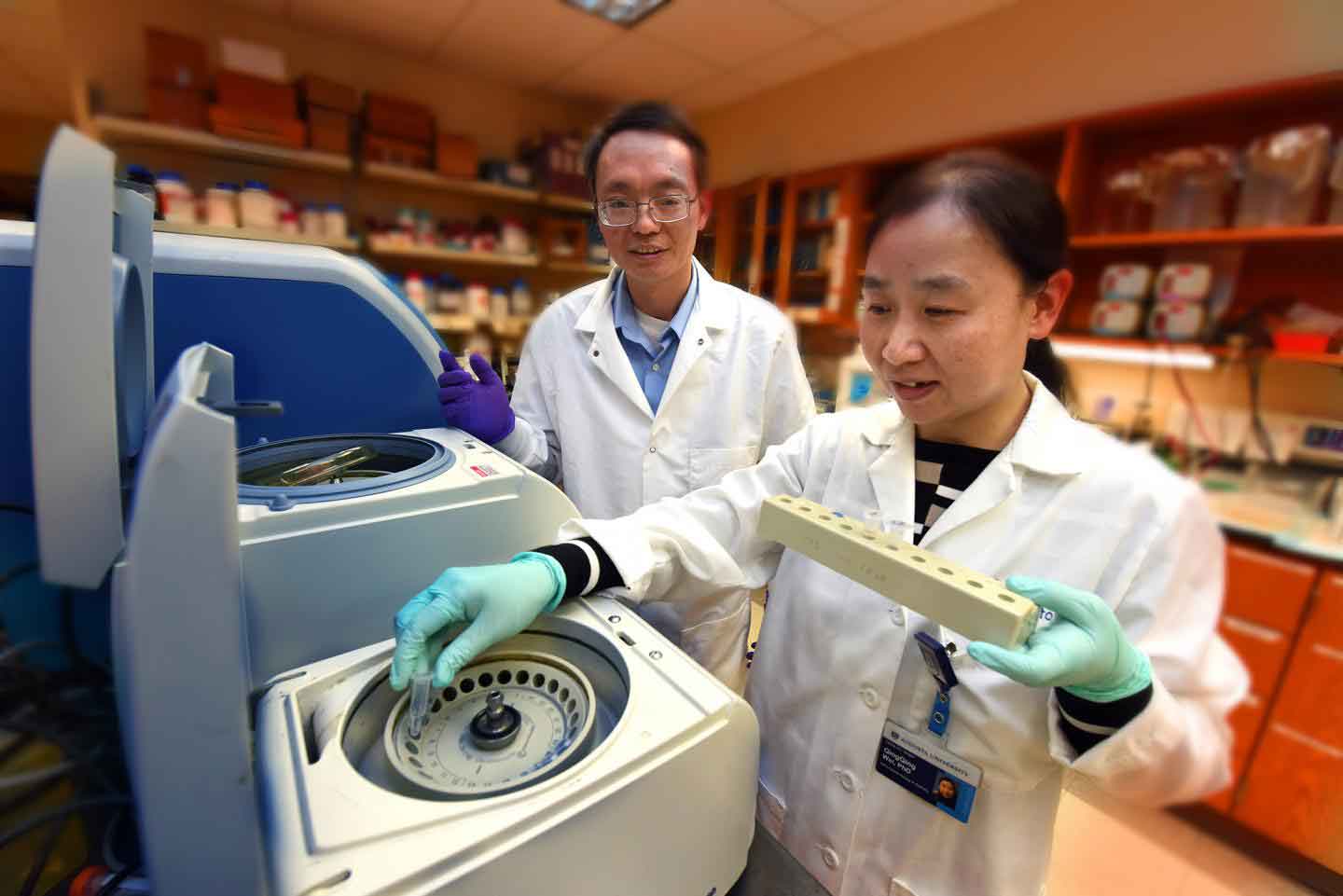
CREDIT
Phil Jones, Senior Photographer, Augusta University
Scientists started from studying a large number of microRNAs. A microRNA-668 is found to be elevated in both patients with an acute kidney injury.
The balance between Mitochondrial fission and fusion is key to a healthy cell powerhouse. Both are monitored by two distinct classes of proteins, which emerging evidence suggests are regulated by microRNAs.
Proteins like mitochondrial Protein 18 KDa, or MTP18, for instance, have just been involved in powerhouse fission, in any event in times of pressure. The MCG researchers and their partners have now affirmed it’s an immediate focus of microRNA-668.
However, the pathway has somewhere around one prior purpose of activity: hypoxia-inducible factor-1, or HIF-1, an interpretation factor that increments when oxygen levels decline to enable cells to change by controlling articulation of qualities that can ensure them.
They found that ischemic intense kidney damage incites HIF-1, which upregulates microRNA-668, which suppresses MTP18 and the outcome is kidney cell protection.
Dong said, “The microRNA-668 gene is a new targeted gene for HIF-1, which may help explain some of HIF-1’s protective function.”
Restricting microRNA-668 leads to the death of kidney cells. Conversely, giving a mimic of microRNA-668 – to increase its presence – protected kidney cells. More microRNA-668 also meant less MTP18 and vice versa.
This gives scientists an idea that MTP18 does when stressed. It induces fragmentation of the mitochondria. They found that increased levels of microRNA-668 can prevent most of that damage so the cell can keep functioning ideally until blood and oxygen are restored.
One way physicians might one day improve the odds for mitochondrial and kidney survival may be a class of drugs called PhD inhibitors, which have already been studied in chronic kidney disease. PHD – prolyl hydroxylase – is a protein that induces the degradation of protective HIF-1 and Dong suspects PHD inhibitors could benefit patients with acute kidney injury as well. A microRNA-668 mimic, similar to that used in the studies, might one day be another option.
The study is published in the Journal of Clinical Investigation.
