By using a new live artificial nerve tissue, scientists at the UCL, ReNeuron and Sartorius Stedim Biotech have successfully repaired severe nerve damage. Scientists now hope that the tissue could possibly open up universal therapy to improve the treatment of peripheral nerve injuries by removing the need for nerve grafts which cause additional damage and personalized stem cell therapies which take weeks to prepare.
Dr. James Phillips, the lead study author said, “Peripheral nerve damage can be severe and extremely debilitating, causing a loss of sensation or movement and the possibility of chronic pain. It is often as a result of trauma from road traffic accidents and frequently affects young people at huge personal cost.”
The investigation, distributed today in Scientific Reports and subsidized by Innovate-UK, demonstrates a quantifiable recuperation of engine and tactile capacity in harmed rodent nerves repaired utilizing the fake tissue as a scaffold between two disjoined nerve closes.
Right now, there are no built cell treatments to treat nerve harm and where vast holes exist in harmed nerves, joins are taken from a sound piece of the body to repair a more vital capacity. For instance, a nerve that gives a tactile capacity in the foot might be utilized to repair development in the arm.
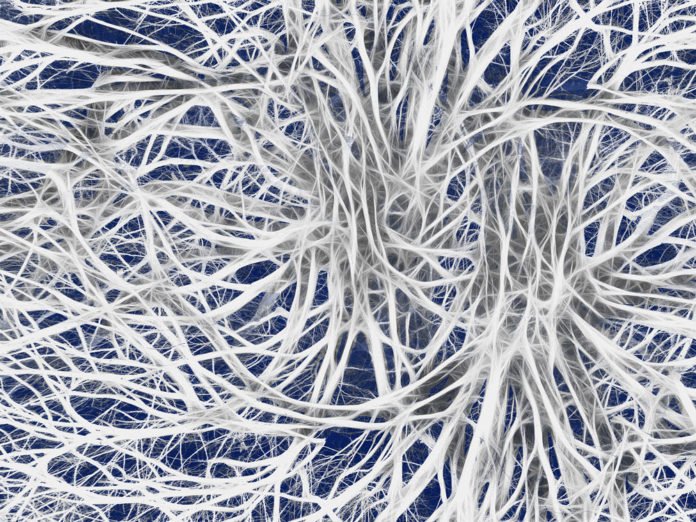
The recently created living counterfeit nerve tissue (called Engineered Neural Tissue, EngNT-CTX) is made of ReNeuron’s CTX clinical review human neural undifferentiated cells produced to GMP measures and adjusted inside a collagen hydrogel sheet. This living tissue is moved into tubes that are utilized to connect the holes in nerves. As the material is allogeneic, it can conceivably be utilized as a part of anybody.
ReNeuron’s CTX cells are now being tried in clinical trials for the treatment of inability coming about because of ischaemic stroke yet this is the first occasion when they have been joined with a built help to control nerve repair in vitro and in vivo.
For the examination, rats with sciatic nerve wounds were treated with either EngNT-CTX sheets conveyed in collagen tubes, an autologous nerve join – the present treatment utilized as a part of doctor’s facilities today – or discharge collagen tubes.
Following two months, the treated nerves were evaluated utilizing an assortment of techniques to test their capacity and development. EngNT-CTX develops were practically identical to autologous nerve unites in supporting adequate nerve recovery to re-setup useful associations, and electrophysiological investigations of muscle work gave a more grounded reaction from nerves repaired with EngNT-CTX contrasted with the autologous nerve join and the vacant collagen tubes.
Dr. Phillips said, “We’re impressed with how well the living artificial nerve tissue performed against the autologous nerve grafts. Although it is only in an animal model, it demonstrates that nerves can be repaired using engineered living constructs and opens up possibilities for future treatment options for repairing severe nerve damage.”
“The generation of artificial nerve using cells to replace autografts for peripheral nerve repair has relied on bespoke procedures using autologous cells and individualized matrix, permitting very limited and expensive clinical application. Combining the Phillips group’s self-aligning collagen technology using ReNeuron’s allogeneic, clinically validated CTX neural stem cells along with simple production methodologies, represents a step forward in developing a more readily available clinical product at reasonable cost.”
Professor Martin Birchall said, “Many patients undergoing nerve repair for trauma or after cancer surgery are not fully served by conventional repairs which may lead to slow and inaccurate regrowth. The development of a targeted, stem-cell based repair product, available to all surgeons, especially in the emergency setting, would represent a massive breakthrough in care. These preliminary studies provide considerable optimism that Eng-NT might, literally and metaphorically, fill this gap.”
Mr. Tom Quick said, “This is exactly what clinicians have been hoping for. This project is clearly focused on delivering the key clinical unmet need in surgical treatment- the nerve gap. A solution like this will address the question successfully and will allow us to treat a nerve gas to the patient’s benefit.”