Lung cancer is the leading cause of cancer death. Survival rates for metastatic lung cancer, including non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC), are poor.
Immunotherapy uses medicines to help a person’s immune system recognize and destroy cancer cells more effectively. Historically, immunotherapy has had minimal success in lung cancer, resulting in the common belief that lung cancer is nonimmunogenic.
Why the immune system mounts such a lackluster response to lung cancer, even after treatment with immunotherapy drugs?
A new study from MIT has shed light on this. In a mouse experiment, the scientists found that the bacteria usually present in the lungs contribute to the environment that inhibits T-cell activation in the lymph nodes near the lungs. There is no presence of the kind of immune-suppressive environment in lymph nodes near tumors growing near the skin of mice.
Stefani Spranger, the Howard S. and Linda B. Stern Career Development Assistant Professor of Biology, a member of MIT’s Koch Institute for Integrative Cancer Research, said, “There is a functional difference between the T-cell responses that are mounted in the different lymph nodes. We’re hoping to identify a way to counteract that suppressive response so that we can reactivate the lung-tumor-targeting T cells.”
Cancer cells send immunosuppressive signals, prompting T-cell exhaustion. Immunotherapy is set to restore those T cells so they can begin attacking tumors again.
In the case of Lung cancer, some T cells stop working even before they reach a tumor because of a failure to become activated early in their development. This activation failure occurs in the lymph nodes, which filter fluids that drain from nearby tissues.
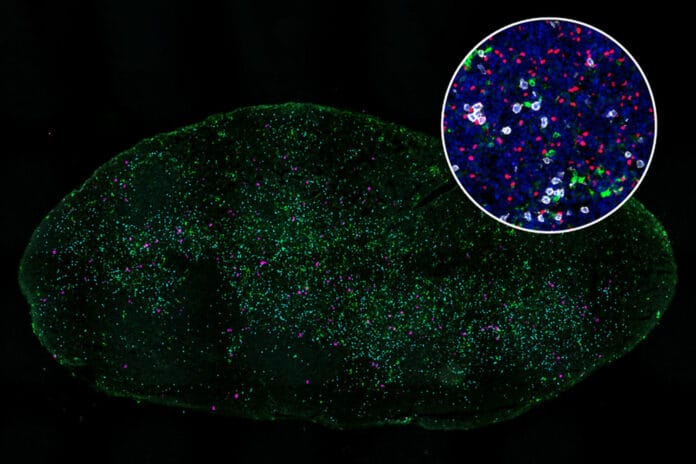
The study examined mice that had tumors implanted either in the flank or the lungs to understand better why some killer T cells fail to function as intended. All of the tumors were genetically identical.
The scientists found that T cells did interact with dendritic cells in lymph nodes that drain from lung tumors and detect the tumor antigens those cells express. However, due to inhibition by a different population of T cells known as regulatory T cells, these T cells could not fully activate.
The lymph nodes that drain from the lungs saw a substantial activation of these regulatory T cells, whereas lymph nodes next to tumors in the flank did not. Normally, regulatory T cells prevent the immune system from attacking the body’s cells. But the scientists also discovered that these T cells obstruct dendritic cells’ capacity to activate killer T cells that specifically target lung cancers.
Scientists also discovered how these regulatory T cells suppress dendritic cells: by removing stimulatory proteins from the surface of dendritic cells, which prevents them from being able to turn on killer-T-cell activity.
Spranger says, “Interferon gamma has a variety of effects on immune signaling, and blocking it can dampen the overall immune response against a tumor, so using it to stimulate killer T cells would not be a good strategy to use in patients.”
Scientists are now exploring other ways to help stimulate the killer T-cell response, such as inhibiting the regulatory T cells that suppress the killer T-cell response or blocking the signals from the commensal bacteria once the researchers identify them.
Journal Reference:
- Maria Zagorulya, Leon Yim, et al. Tissue-specific abundance of interferon-gamma drives regulatory T cells to restrain DC1-mediated priming of cytotoxic T cells against lung cancer. Immunity. DOI: 10.1016/j.immuni.2023.01.010