Are hypertension and blood pressure change in early adulthood associated with late-life brain health, and is there variation by sex?
A new study by UC Davis assessed the association of early adulthood hypertension and blood pressure (BP) change with late-life neuroimaging biomarkers and examined potential sex differences. Scientists compared MRI brain scans of older adults who had high blood pressure between the ages of 30 to 40 with older adults who had normal blood pressure.
The high blood pressure group had significantly lower regional brain volumes and inferior white matter integrity, according to the study’s findings. Both elements have a connection to dementia.
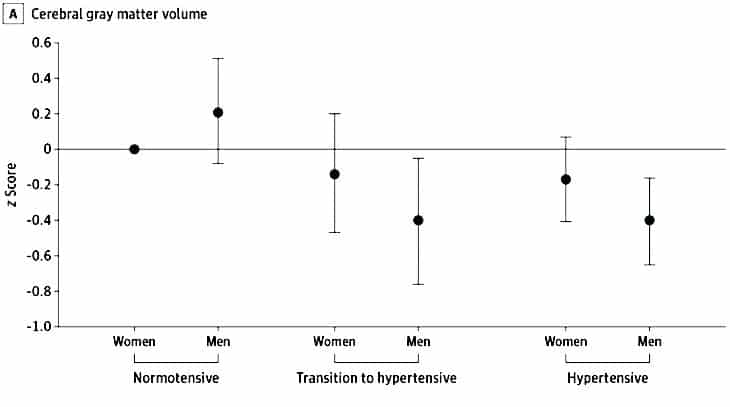
The study also revealed that men had more pronounced unfavorable changes in different brain regions than women, such as reduced frontal cortex volume and grey matter volume. They mention that the differences might be connected to estrogen’s premenopausal protective effects.
First author Kristen M. George, an assistant professor in the Department of Public Health Sciences, said, “Treatment for dementia is minimal, so identifying modifiable risk and protective factors over the life course is key to reducing disease burden.”
“High blood pressure is an incredibly common and treatable risk factor associated with dementia. This study indicates hypertension status in early adulthood is important for brain health decades later.”
The Study of Healthy Aging in Black Americans and the Kaiser Healthy Aging and Diverse Life Experiences (KHANDLE) study contained data on 427 participants (STAR). This gave them access to health information for a diverse cohort of older Asian, African, Latino, and white adults from 1964 to 1985.
The individuals’ blood pressure was measured twice when they were between the ages of 30 and 40. By doing so, they could identify whether their blood pressure had been normal during their adolescence, was on the verge of being normal, or had been hypertensive.
They also looked at MRI scans of the participants conducted between 2017 and 2022. The scans allowed them to look for late-life neuroimaging biomarkers of neurodegeneration and white matter integrity.
Those with high blood pressure or those transitioning to it showed lower cerebral grey matter volume, frontal cortex volume, and fractional anisotropy in their brain scans compared to those with normal blood pressure (a measure of brain connectivity). Men with high blood pressure received lower scores than women with the same condition.
Rachel Whitmer, professor of departments of Public Health Sciences and Neurology, said, “This study truly demonstrates the importance of early life risk factors and that to age well, you need to take care of yourself throughout life — heart health is brain health.”
“We are excited to be able to continue following these participants and to uncover more about what one can do in early life to set yourself up for healthy brain aging in late life.”
Journal Reference:
- Kristen M. George, Pauline Mailard et al. Association of Early Adulthood Hypertension and Blood Pressure Change With Late-Life Neuroimaging Biomarkers. JAMA Netw Open. DOI: 10.1001/jamanetworkopen.2023.6431
