Patients with type 2 diabetes can’t adequately control their glucose levels. The most normally endorsed sedate is called metformin, however in the event that this doesn’t work, or triggers reactions, patients are generally offered different medications. These incorporate a class of medications called “incretin mimetics”, which animate the arrival of insulin from particular cells in the pancreas, called beta cells.
According to a new study by the Imperial College London, suggests that rolling out small improvements to existing diabetes medications can adjust how they collaborate with cells, and conceivably make the drugs more compelling.
The method enables scientists to hack into the ‘traffic system’ that shuttles drugs in and out of cells. This tends to increased efficiency of the drug.
Scientists in the study mainly focused on one of these aggravate, a medication called exenatide, which patients infuse twice-day by day or week by week, contingent upon the definition. The compound demonstrations by official to and enacting a kind of docking point – called GLP-1 receptors – found on the surface of beta cells, which fortify the phones to discharge insulin.
Scientists explained how exchanging a couple of the building squares of exenatide could create new mixes with marginally extraordinary properties, changing how they communicate with the GLP-1 receptors and making the medications more successful.
Dr Ben Jones, from the Bloom Lab at Imperial said, “Under normal conditions, we may not want cells to be continually activated, so these receptors are internalized and no longer accessible to naturally occurring GLP-1 outside of the cell. However, when you have a disease where we can get benefit from continual stimulation of receptors, then avoiding this internalization process could be an advantage.”
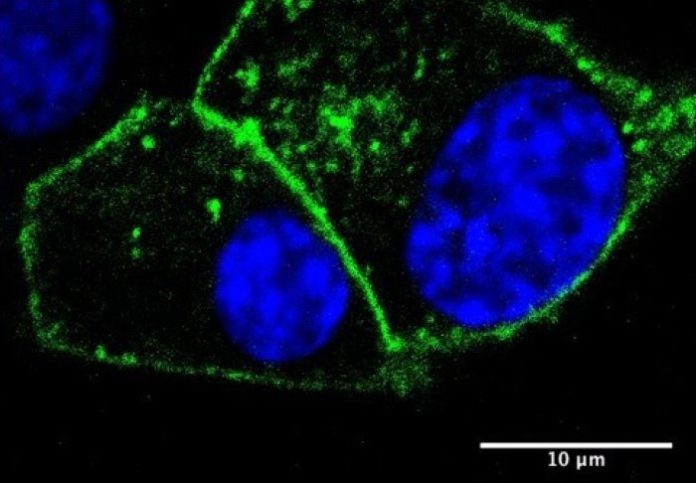
The team found that one of their mixes, called “exendin-phe1”, modified the GLP-1 receptor trafficking process. In trials with human beta cells in the lab, they found that their compound lessened how much the receptors left the layer, prompting more receptors accessible on the cell surface to tie to the medication.
With the standard treatment, an expected 90 for each penny of GLP-1 receptors would move from the film into the cell, with just around 10 for every penny being reused. With the new compound, be that as it may, only 30 for each penny of the receptors moved into the cell and the lion’s share of those was reused, coming back to the cell layer.
In mouse contemplates, the scientists found that while their new compound expanded the measure of insulin being discharged from the creatures’ beta cells in the pancreas, it seemed to have no expanded impact on GLP-1 receptors somewhere else in the body – to be specific GLP-1 receptors in the mind, which are related with nausea.
Tweaking medications to impact receptor trafficking could prompt enhancements for a large group of existing medicines. For instance, morphine can give relief from discomfort by focusing on opioid receptors in the body, yet it can have various off-target impacts, including stoppage and other gastrointestinal impacts, and additionally discouraging the respiratory framework.
By changing the structure of opioid medications to modify receptor “inclination” (a wonder identified with trafficking), scientists have possessed the capacity to lessen these impacts, while keeping up the torment easing properties of the medications.
The Imperial group is currently arranging a little report with solid human volunteers to additionally investigate the component of receptor trafficking and how it could be utilized, which is relied upon to start inside the coming months.
Dr Alejandra Tomas, a Lecturer in Professor Guy Rutter’s Section and co-senior author of the study, said: “We have found that making small changes to drug molecules can dramatically alter receptor trafficking. Ultimately, we’re interested in using these compounds as tools to try and understand receptor biology and generate even more effective drugs in the future.”
The study is published in the journal Nature Communications.